
In this 29th episode of the Sports MAP Podcast we chat with Lead Physiotherapist of the Matildas, Australian Womens Football Team, Jaclyn Benz. Jaclyn has immense experience working at all levels of womens football. Her experience extends well beyond Women's Football after spending timeworking as a Locum at the Australian Institute of Sport and Hunter Sports Academy.
In this episode we cover a range of topics including:
- Jaclyn's background and pathway to her current position
- Her day-to-day experience of the recent World Cup
- Training and prep for the World Cup campaign
- Individualising injury prevention programs
- Injury differences between womens and mens sport
- Challenges and opportunities within womens elite football
- Management of Sam Kerr's calf injury
- Pressures and celebrations throughout the World Cup campaign
Listen to this Podcast via your favourite platform including Apple, Spotify, Player FM & Stitcher.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook
For contact sport athletes, a common injury which is prevalent is an injury to the Medial Collateral Ligament (MCL) of the knee. As a diagnostic and rehabilitation professional, it is important to understand the mechanics of the anatomy of the MCL in order to accurately diagnose the injury and the recondition an athlete back to their full performance capacity. The purpose of this blog will be to outline the epidemiology of isolated high grade MCL injuries; differential diagnosis and the rehabilitation process from Protection to Return to Performance utilising a systems based approach that can be applied to multiple knee pathologies.
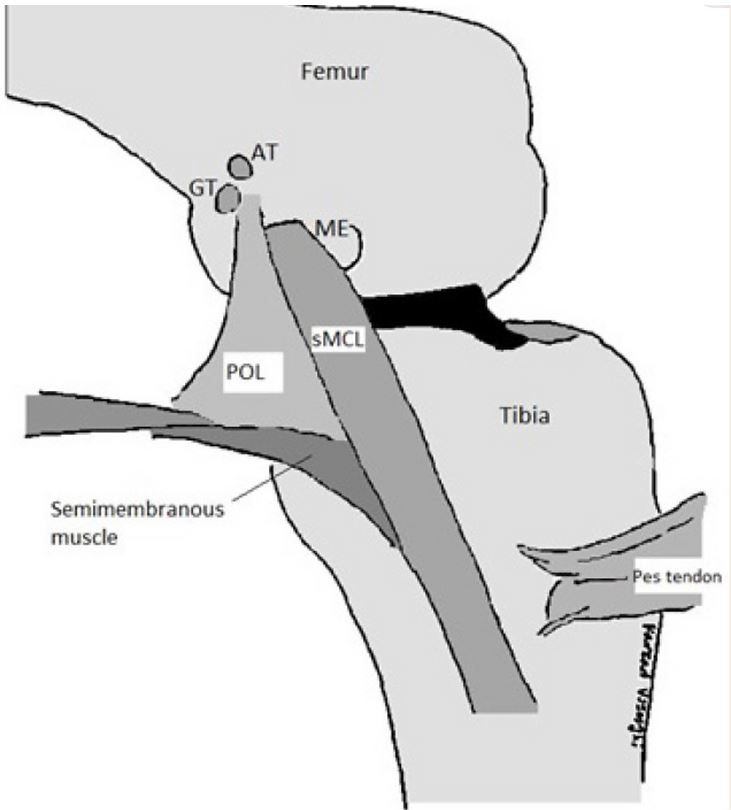
Anatomy & Function of the MCL
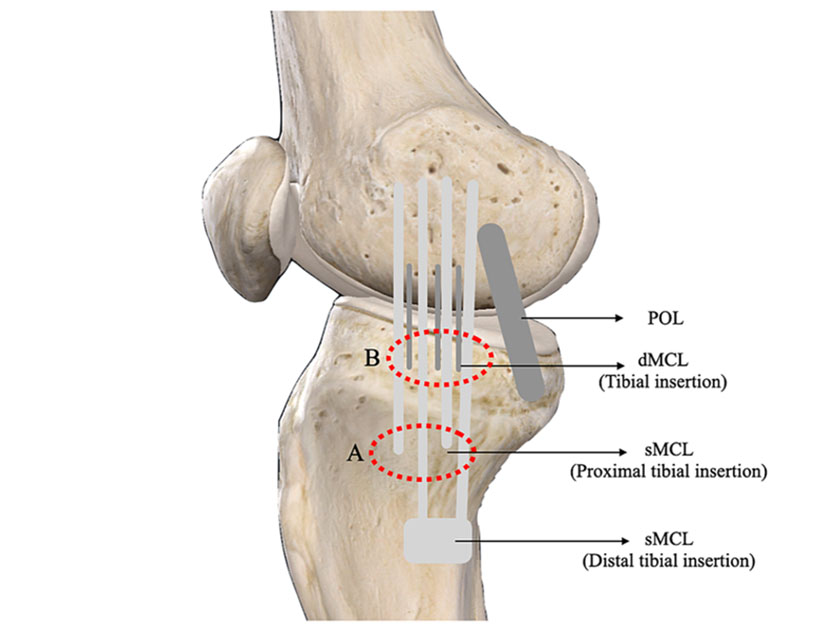
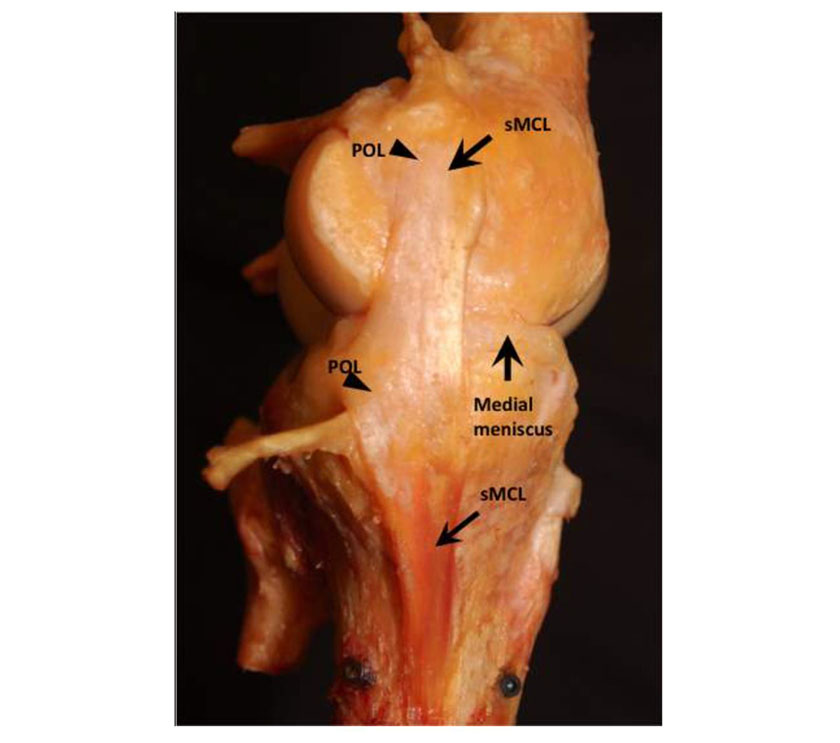
Crucially it is important to understand that the MCL is composed of two distinct bands that allow it to perform its anatomical role. These are known as the Superficial MCL (sMCL) and the Deep MCL (dMCL). The superficial and deep ligaments each have a unique function, making the MCL the primary responder to valgus stress and a secondary restraint to rotational forces. The sMCL, specifically the proximal division, resists valgus forces through all degrees of knee flexion. The distal division of the sMCL helps stabilize external rotation of the knee at 30-degree flexion. The dMCL helps stabilize internal rotation of the knee from full extension through 90-degree flexion (Juneja et al 2022).
The sMCL has its proximal insertion at the medial epicondyle of the femur where it blends into the semimembranosus tendon. The distal attachment is at the posteromedial surface of the tibia. The dMCL is composed of 2 ligaments: meniscofemoral and meniscotibial. The meniscofemoral has its proximal insertion at the femur just distal to that of the sMCL; it attaches to the medial meniscus. The meniscotibial ligament is thicker and shorter. It travels from the medial meniscus to the distal edge of the articular cartilage of the medial tibial plateau (Juneja et al 2022).
Mechanisms of Injury: Contact vs Non Contact
When placed in a situation that an athlete has suffered an acute injury and pain to the medial aspect of their knee, it is important to decipher whether the primary mechanism of injury (MOI) is either contact or non contact. For isolated MCL injuries, ~80-90% of them come from a contact MOI whereby a Valgus stress occurs. In field / court based contact sports, due to the position of the knee and the force vectors, a combined flexion/valgus/external rotation injury is usually the end result. The vast majority of MCL injuries are from a direct blow to the outer aspect of the lower thigh or upper leg (Phisitkul et al 2006). The exception to this is in winter sport athletes such as skiiers who have high rotation loads when cutting and turning. In light of this, if an athlete is subject to a non contact MOI and presents with MCL laxity, a suspicion must be present for a concurrent ACL injury regardless of clinical testing results for the ACL itself.
Immediate Assessment & Management
When determining the grading of an isolated MCL injury, there is a wide variety of presentations that a clinician can be faced with. Particularly important is the athletes natural level of laxity and thus stress test comparisons with the non injured limb is critical to providing an accurate assessment. Gradings for an injury to the MCL can be defined as the following:
Grade 1 - Pain on stress testing at 0 & / or 30 degrees with nil significant laxity in comparison to the contralateral limb
Grade 2 - Pain on stress testing 0 & / or 30 degrees with comparable laxity in comparison to the contralateral and a presence of a ligamentous end feel
Grade 3 - Pain or no pain on stress testing 0 & / or 30 degrees with significant laxity in comparison to the contralateral and no end feel.
Palpation is an important tool in conjunction with radiographic imaging in determining whether the injury has been sustained to either of the: Femoral component; mid belly MCL or Tibial component of the ligament. Prognosis can differ with slower recoveries indicated for injuries to the tibial insertion of the MCL due to it's thinner anatomical insertion
As this blog is dedicated towards a high grade injury, when a grade 2 and above injury is suspected, the clinician should place the athlete in a hinged knee brace restricting the athlete from end ranges of extension and flexion that place higher strain on the MCL (Vosoughi et al 2021). Conjecture exists surrounding the natural history and recommendations for bracing, there are no set rules on how long an athlete should be braced for and a principle that I like to live by is that an athlete will remain braced until the ligament stabilises. An example 6 week bracing progression is listed below
Weeks 1 & 2: 30 - 60 degrees
Week 3: 20 - 70 degrees
Week 4: 10 - 80 degrees
Week 5: 0 - 90 degrees
Week 6: 0 - 120 degrees
Week 7: Brace off
Importantly, a clinician should not regularly assess healing of the MCL as this may disrupt fibres that are attempting to scar and realign. Personally I re-assess the MCL at the week 4 mark after initial collagen has had time to be laid and then at 2 week intervals until it has stiffened up to the comparable marker of the contralateral limb.
*A clinical observation I have made is that assessment at 0 degrees of extension stabilises and reduces in irritability far faster than at 30 degrees of flexion.
Radiography: What value can it add?
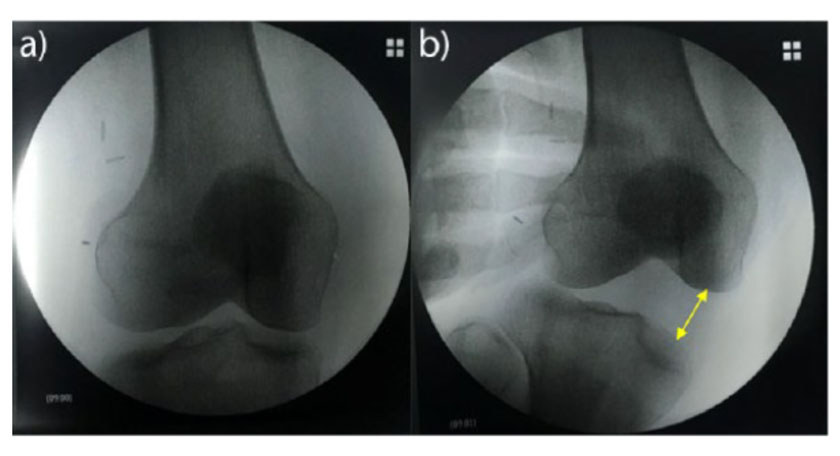
As mentioned above, radiography can assist with a clinical diagnoses in many ways:
-
In the presence of non contact injury confirm Dx for concomitant pathology
-
Confirm clinical grading of MCL injury
-
Confirm location of MCL injury
Different methods of radiographical assessment exist, namely through the form of valgus stress x rays or MRI. I havn't come across a scenario where valgus stress x rays are practical so in that space MRI imaging should be ordered.

Rehabilitation Planning:
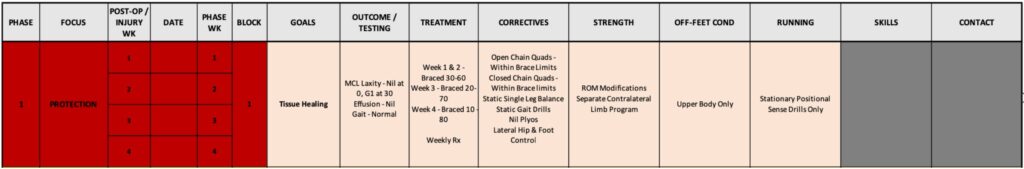
Importantly, part of my process for any long term rehabilitation planning is to map out the projected journey from start to finish and break it down into our 5 phases of rehabilitation that we utilise at Athletes Authority.

By detailing the rehabilitation plan it allows myself as the clinician to be targeted and objective my staged progression as well as giving the athlete context to each mini progression and goal that we tick off along the way. Below is an example of a full detailed rehabilitation plan for a high grade isolated MCL injury.
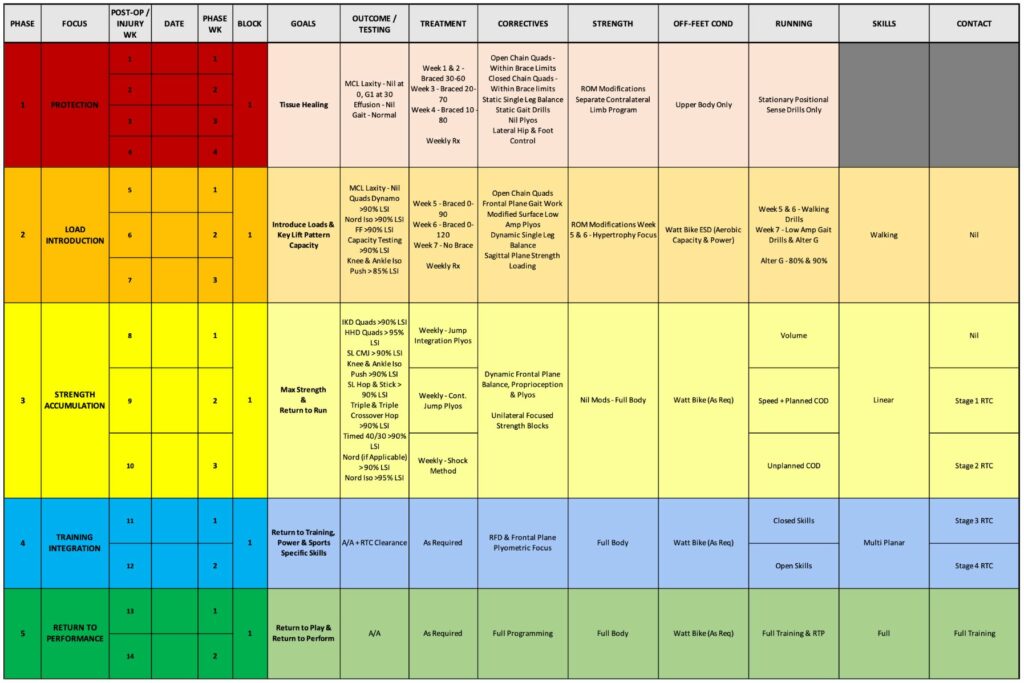
Important key themes within the progression of the rehabilitation plan include the restoration of physiology in the Protection phase. Development of base strength capacity in the Load Introduction phase. Restoration of plyometric capacity, particularly within the frontal plane in the Strength Accumulation phase; in tandem with return to run. Late stage return to contact and skill demands in the Training Integration & Return to Performance phase.
Following on from this macro rehabilitation plan, I then look to design integrated training weeks with the athlete in the form of a micro weekly rehabilitation plan. This allows for appropriate measures of load monitoring and session timing when designing a program that encompasses for local tissue restoration; full body strength capacity & cardiovascular reconditioning.
Whilst giving complete insight into an athletes full journey is impractical deliver on a blog, below I will outline some key training program progressions that could be utilised in different phases of the rehab journey.
Protection Phase:
Within the protection phase, our primary focus is to facilitate an environment that allows the MCL to gain strong foundations of anatomical healing and scar formation. First and foremost ensuring that the hinged ROM brace provided to the athlete is fitted correctly and that compliance is maintained to wearing the brace is priority number 1. I have experienced scenarios in the past whereby I felt my rehabilitation planning and implementation was incredibly spot on however once we got to clinical re-assessment date it came to my surprise that there was still significant laxity in the ligament. Upon further questioning I would then discover compliance with the brace had deteriorated because the athlete felt it was impacting their ability to perform their rehabilitation. Ironically, this desire to improve their rehab became their downfall. An important lesson for me to learn and a reminder that in rehabilitation, the basic principles of tissue healing come before those of strength & conditioning restoration.
With this in mind, second order principles are the following:
-
Reduction of pain & swelling
-
Re-activation of Quadriceps
-
Maintenance of Hamstring, Calf & Foot strength
-
Development of single leg stance and lateral hip rotation control
-
Energy Expenditure
Reduction of pain & swelling:
Despite a lack of concrete evidence existing for the efficacy of cryotherapy against reduction in localised inflammation post injury, there remains a strong level of evidence for the use of cryotherapy in the improvement of function post severe trauma to the knee (Dambros et al 2012). My preference in clinic is to utilise Game ready protocols of 30 minute sessions whenever the athlete is in the facility, before and after they perform their rehabilitation. Analgesic effects provided from cryotherapy can reduce arthrogenic muscle inhibition (Rice et al 2009) as well as providing improvements in joint range of motion (Dambros et al 2012, Rice et al 2009). For maintenance at home, I would provide a compression sleeve for the athlete to wear in conjunction with regular icing whenever they are sedentary at home.
Amongst passive protocols, it is important for an athlete to maintain an active approach to this process. Utilisation of the skeletal muscle pump in the lower limbs can be an effective way of clearing fluid, particularly as in the instance of a high grade injury and that the MCL is an extracapsular structure, swelling may pool well below the knee into the calf and ankle.
Simple protocols such as ankle pumps can be scaled effectively to an athlete wearing a brace, can be done anywhere and place no undesired load onto the healing MCL.
Re-activation of Quadriceps:
Acute trauma and associated joint swelling are key contributors to arthrogenic muscle inhibition of the quadriceps. AMI is caused by a change in the discharge of articular sensory receptors whilst the importance of the quadriceps to overall knee function surrounds the relationship between skeletal muscle and their role in providing shock absorption towards articular joints (Suzuki et al 2022).
Key principles are to develop quadriceps strength within the allowances that the hinged ROM brace provides to the athlete. A high variability in athlete function can exist within this population and it is important to achieve a stimulus that is great enough to overcome aforementioned AMI and redevelop quadriceps capacity. Having a continuum of early stage exercise progressions is critical in being able to apply the appropriate progressions towards the athlete in front of you. Below are some examples of protection phase quadricep focused options that you may utilise with an athlete.
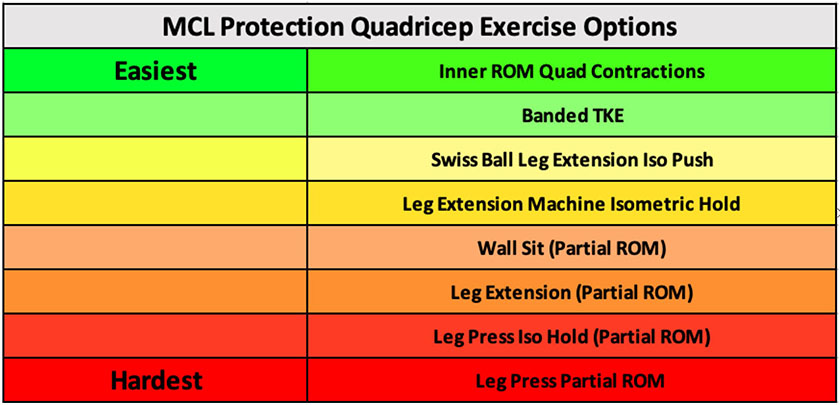
Below are three examples of early stage protection phase quadricep exercises. I normally combine all of these with NMES and BFR for increased neural drive and metabolic stress production.
Maintenance of Hamstring, Calf & Foot Strength:
Whilst quadriceps are the key priority in the early stages of rehabilitation, the importance of the hamstrings, calves and feet are paramount in ensuring optimal functional rehabilitation once an athlete enters a more integrated pattern of movement demands. As discussed in a previous blog (https://www.sportsrehab.physio/post/failure-of-hamstring-graft-aclr-part-1-the-role-of-eccentric-strength); the hamstrings play an intricate role in the protection of knee health, whilst the calf and feet are gaining increased attention due to it's role in force production, absorption & neuromuscular control when running (Bohm et al 2021).
A consideration for the rehabilitation professional when it comes to hamstring exercise prescription is the interrelationship between the MCL and the insertion of the distal hamstrings at the pes anserinus (Vosoughi et al 2021). During knee joint flexion, the semimembranosus muscle contracts and tightens the posteromedial knee capsule and the POL. It also pulls the medial meniscus posteriorly and prevents the anterior subluxation of the tibia. Another important role of the semimembranosus muscle is internal rotation of the tibia (Vosoughi et al 2021). Matching this with literature suggesting that exercises such as lying leg curls may preferentially activate the medial hamstrings in comparison to the lateral hamstrings (Bourne et al 2017) the rehabilitation professional should monitor with caution patient responses to traditional concentric based hamstring exercises.
With this anatomical consideration in mind, my hamstring based progressions typically are centred around the projected load that I believe will be placed on the posteriomedial corner (PMC) of the knee. Below is an example exercise progression based around this concept with some notes on progression of exercise options. It is important to note that progressive overload should be kept front and centre in mind as the athlete recovers and we can utilise increased loading and volumes in conjunction with more challenging exercise progressions

When evaluating options for the foot and calf, my focus is on increasing the force production of the Gastrocnemius and Soleus musculature whilst improving the proprioceptive capacity of the foot intrinsics, extrinsics and ankle stabilisers. As stated above, options should be scaled to the athletes level of competency and function whilst what also should be kept in mind is that they will be bound to the ROM restrictions of a brace so expectations should be that particularly for calf based options that the soleus will end up with greater loading than the gastrocnemius in this phase of rehab.
Below are some examples of accessory foot and calf options that I typically prescribe:

Development of Single Leg Stance & Lateral Hip Control
An area I wouldn't place a large deal of emphasis on early however is pivotal during the back end of protection and during the load introduction phase. Primary reasoning for me behind not placing it as a priority (at least in functional positions) early in rehab is due to the fact that the athlete will be stuck in a position of mini knee flexion and thus prolonged time loading in single leg stance may lead to overload of the patellofemoral joint. Nevertheless an example stream that may assist in the development of the lateral hip has been placed below for consideration.

Energy Expenditure:
One of the biggest issues that athletes face when they are compromised of their usual training routine is that metabolically they face an imbalance of calorie in and calorie out energy expenditure. Whilst the purpose of this blog is not to discuss the ins and outs of energy intake requirements during rehabilitation (which is generally higher to support tissue healing) and that certain supplementation may assist in recovery (I'll leave this to my Dietitian friends), when an athlete suddenly loses their greatest contribution of energy output in their team training it can be useful to substitute this with off leg conditioning options.
Something I find important to stress is that particularly in the early stages of rehabilitation when an athlete is completely leg compromised when it comes to cardio training options, we shouldn't expect much development when it comes to higher end aerobic adaptation due to the inability for the athlete to reach Vo2 Max when it comes to upper body only cardiovascular training. In this light I like to keep Intervals short, Intensities high and recovery low.
A sample session I like to utilise is very simply a 20/10 Tabata interval session x 8-10 reps x 2-4 sets at the end of an athletes strength training session. Similarly, placing time caps on an athletes strength component of their sessions can increase overall metabolic output through decreasing rest periods between sets.
Load Introduction Phase:

With solid foundations laid in the Protection Phase, my key foci in the Load Introduction Phase are namely to increase the intensity of the strength training that has been established in the protection phase; increase ROM allowances and transition the athlete towards more functional, unilateral training and most importantly; introduce plyometric and modified surface running demand.
When it comes to progressing an athlete in quad dominant lifting exercises, my preference is to transition athletes from Bilateral --> Unilateral Oriented --> Unilateral progressions. Namely due to the demands that unilateral closed chain training places on valgus control on the knee. Hypothesising decreased proprioceptive control during the initial stages post healing, it makes sense to me to develop proficiency with an increased base of support prior to moving on to true unilateral streams.
As the athlete shifts into more functional lifting, combination cueing can be utilised such as medially banding split squats to further constrain the athlete and force greater deep gluteal external rotation and abduction activation to prevent valgus force on the knee.

Developing a Performance Profile
Once an athlete has full terminal extension, nil effusion, a solid end feel on clinical testing and 80% quadricep, hamstring and calf strength capacity; this is enough for me to commence low amplitude plyometrics.
Assessment procedures I utilise are via the VALD Performance Dynamo for quadricep testing, VALD Performance Nordbord & Forcedecks for Hamstring testing as seen in a seperate blog (https://www.sportsrehab.physio/post/assessment-of-hamstring-strength-post-aclr) and a combination of VALD Performance ForceFrame & ForceDecks for maximal straight knee and bent knee calf torque. These maximal torque tests are performed in conjunction with capacity based endurance testing of single leg squats, single leg foot elevated hip bridges and single leg straight knee & seated calf raises.
When creating a velocity profile for the athlete, I believe it is important to get an idea on how an athlete produces force both bilaterally and unilaterally as well as in horizontal and vertical vectors. This is largely centred around the altering contribution of the hip, knee and ankle in the propulsion and landing phases of both horizontal and vertical jump tasks (Kotsifaki et al 2021; Kotsifaki et al 2022).
A full list of assessments that I utilise to begin my performance profiling in the load introduction phase is displayed below:

Redeveloping Plyometric Capacity:
As an introduction to low amplitude plyometrics, similarly to my strength progressions I progress the athletes from Bilateral --> Unilateral Oriented --> Unilateral Tasks. I find Pogo jumps to be incredibly versatile in this space and an excellent precursor to shifting athletes towards more specific skipping based drills which are effective in promoting the 'bounce' component of the Max Velocity phase that we want to see in an athletes running.
Below are some examples of progressions from bilateral to unilateral low amplitude plyometrics:
One important bug bear of mine to note is that when I see athletes performing pogo variations, a common error I see is far too much knee flexion when the athlete hits the ground. This is not only inefficient in the sense of increasing ground contact time and shifting energy up the kinetic chain, it can also lead to overload of the PFJt. When prescribing pogo jumps, the objective is to gain maximal output from the calf-achilles complex and thus cueing strong active dorsiflexion when in the air, plantarflexion to hit the ground hard and maintain stiff knees is critical.
In addition to low amplitude plyos, I believe in the Load Introduction Phase we can also expose the athlete to a good base of eccentric absorption type plyometric progressions to assist in increasing the athletes eccentric rate of force development (RFD) in their quadriceps. Tall to Short and Altitude Landing variations are my preferred go to in this space, however I find that we as professionals typically under load these exercises. My objective is to progress athletes towards loading these with dumbbells and eventually a heavy trap bar in hand
Restoration of Gait Mechanics:
When it comes to restoring an athletes gait mechanics prior to returning to run, I follow a very simple model of stepped progression. This is based around certain positions of athletic movement and then broken into different stages of complexity and intensity.
The athletic positions I place emphasis on are the:
-
Acceleration Position
-
Max Velocity Position
-
Frontal Plane / Lateral Position

Selection of emphasis for these particular positions to train varies pending the injury in question. For an MCL I will place greater scrutiny on the Frontal / Lateral plane position and then look to identify which out of Acceleration & Max Velocity positions that the athlete is at their weakest.
Once a position has been selected then the next stage in the development of drills is to identify at what stage of complexity and intensity the athlete can comfortably manage. For me I break this down into 4 stages:
-
Positional Sense Drills
-
Walking Drills
-
Low Amplitude Drills
-
High Amplitude Drills

Below are some examples of some drills that I may utilise in the Load Introduction Phase with an athlete:
Role of Alter G Running:
I believe where available, anti gravity treadmill running can have a significant role to play both physically and psychologically in the transition from gym based rehabilitation to field based running. In contrast to more longer term rehabilitation such as ACL rehab, in the context of MCL reconditioning I am happy to start at a relatively higher % of body mass (%BM) and to allow the athlete to self select a comfortably jogging speed. Normally I would implement these sessions in the week after the athlete has had their brace removed and prior to them returning to running on the field. I like to see the athlete tick off 3 sessions with a ramped increase in %BM whilst leaving the other parameters consistent. A sample week of sessions could look like the following:
Session 1 --> 5 x 1 min Jog / 1 min Walk @ 80%BM
Session 2 --> 5 x 1 min Jog / 1 min Walk @ 90%BM
Session 3 --> 5 x 1 min Jog / 1 min Walk @ 100%BM
Integration Of ESD? Development of Aerobic Capacity
Whilst the focus in the Protection Phase when it came to cardiovascular training was largely centred around energy expenditure, development of Aerobic Capacity in the Load Introduction phase will create a framework for on legs conditioning when the athlete returns to running whilst also assisting to break up the monotony that strength training can sometimes give. Prior to an athlete achieving a great enough level of knee flexion that can facilitate Watt Bike conditioning, I will steer towards the ski erg and cue the athlete for a more hinge dominant pulling pattern rather than a squat based pulling pattern. Additional cues for the athlete during these sessions is to focus on consistency of stroke rate and breathing rather than aiming to pull as hard and fast as they can. A sample session which I might prescribe on the ski erg is the following:
Ski Erg Session Sample - 5 x 5 mins @ 75%RPE / 1 min Passive Recovery (PR)
Once an athlete is able to perform Watt Bike based conditioning I will get a measurement of the athletes Maximal Minute Power (MMP) so that I can utilise accurate intensity targets. A sample Watt Bike session is as follows
Watt Bike Session Sample - 5 x 4 mins @ 70% MMP / 2 mins @ 55% MMP
When it comes to weekly prescription, you really need to get a gauge of your athlete as to how much they can commit to their reconditioning program, particularly in amateur and semi professional settings. In these instances I'll aim for ~1-2 sessions per week whilst for the professional athlete I'd aim for ~2-3 sessions per week.
An example Load Introduction Microcycle could look like the following:

Within the above plan we allow for the following sessions
-
3 x High Day Strength Sessions
-
3 x Alter G Sessions
-
0-4 x Low Day Rehab Sessions
-
1-2 x Off Feet Conditioning Sessions
Weekly planning in my opinion has to be completely individualised, as for many factors certain athletes may be able to dedicate and tolerate more or less than others. In light of this there are no rules in this space and session prioritisation has the utmost importance attached to it in environments where athletes can perform limited sessions
Strength Accumulation Phase:

The primary focus that I want to place emphasis on in the Strength Accumulation phase is the athletes return to running as this certainly a cap in the sports rehabilitation field that I feel is present, particularly in the private sector.
In the context of an MCL injury, the demands of running will increase quickly and I'll aim to develop the following in order:
Target 1 - Volume Tolerance
Target 2 - Speed + Planned COD
Target 3 - Unplanned COD (+ Consolidation of the above)
Usually I will aim for ~2 sessions per week and a rough starting point I like to shoot for is 1000m volume for the athletes first running session and then bumping this up to ~40-50% match volume in session two.
In the initial return to run (RTR) week, the volume that the athlete achieves will not produce any great metabolic or speed producing effects, thus the rehab professional should ensure that the athletes technical drilling is performed exceptionally well to ensure that they gain the most out of each session. In terms of linear based running drills these can be broken down into the following focus
-
Cycle - Developing the cyclical action of the lower limbs
-
Switch - Developing the ability to switch limbs in the air
-
Bounce - Promoting a strong yielding capacity of the lower limbs to 'bounce' off the ground.
An example of technical drills in each stream are included below:
Looking at Speed Development in a short time frame, my experience has yielded greatest results when utilising a 'Short to Long' approach starting at higher running intensities rather than the reverse gradually developing the athletes running speed. This approach places a heavy emphasis on an athletes acceleration mechanics & capacity which is a heavily relied upon trait in field sports whilst also reducing the risk of over exposure to high speed run metres HSRm as it limits the athlete from opening up and moving faster than they should.
Resisted accelerations through the form of banded and sled runs can assist the athlete in being exposed to a strong forward lean position whilst also providing a constraint to increase force production.
As the athlete begins to open up to higher speeds, from both a technical and speed management perspective I like to implement 'Wicket' style drills for the promotion of strong front side mechanics as well as ensuring athletes do not move too quickly or over stride, this allows the rehabilitation professional to create as much of. a 'vacuum' environment as possible.
Speed & Agility Progression
When approaching speed progression in rehabilitation via a short to long approach, the objective is to allow the athlete to reach 100% max velocity over a short distance and gradually build their exposure at 100% max velocity over time. In light of this, there may be many 'sub-levels' within the initial stages of speed exposure in order to build an athlete to 100% of their max velocity. A sample speed progression could look like the following:
Stage 1 - 40m Efforts (10m Build - 20m Hold - 10m Decel) [Build from 80-100% MSS}
Stage 2 - 50m Efforts (10m Build - 30m Hold - 10m Decel) [Build from 90-100% MSS}
Stage 3 - 60m Efforts (20m Build - 20m Build - 20m Hold) @ 95%, 100%, 100% MSS
When looking to recondition an athletes change of direction capacity, consideration needs to be made towards the following variables:
-
Tissue implicated by injury
-
Sub-Capacities of COD
-
Degree of COD
-
Planned vs Unplanned
I personally really like to hone my focus on developing the sub-capacities of change of direction prior to implementing a COD task on the athlete. When looking at this I break down a single COD moment into involvement an acceleration moment, a deceleration moment, pre-cut strategy, cutting moment and finally a re-acceleration.

With this in mind, being aware that we have already dedicated a stream to developing acceleration and speed; my primary key focus is to develop an athletes ability to decelerate prior to asking them to cut. To develop deceleration I'll combine both over exertion type drills such as loaded deceleration lunges to develop the athletes ability to eccentrically control their COM via their quads with drills such as planned decel stop runs to instil the behaviour of dropping their COM and shortening their stride prior to stopping (and eventually cutting).
Once I'm confident in my athletes ability to linearly decelerate, then I'll aim to introduce some planned swerving tasks to improve their ability to control rotation at the hips and torso whilst introducing light planned sagittal to frontal cuts in the form of box based drills
The advantage of a sagittal to frontal plane transition is that it forces the athlete in question to develop push off power from their outside leg, which is a precursor to being able to produce an effective sidestep cutting strategy. Common errors I see in 45 and 60 degree cuts is athletes attempting to swerve and using a crossover step strategy to complete the cut. Whilst this is effective from a safety perspective, I don't personally believe it is practical to expect this to carry over to their return to match play.
Progressing past box drills, this is where my focus will shift to the prescription of <90 degree cuts, with the aim of carrying over the body positioning, lateral pushing power and deceleration strategy into these more dynamic and faster paced cuts. Example drills that you can utilise are 'Z' runs and 'Y' drills.
The primary difference between a cut that is <90 degrees in comparison to a cut that is >90 degrees is in the selection of the cut foot. In <90 degree cuts the most effective cut strategy is to load the outside leg through a sidestep type strategy, whilst for those >90 degree the body position strategy should shift to the athletes bodyweight onto their inside leg to project towards the intended direction of cut. An example of a >90 degree cut drill is displayed below:
Adding elements of reactivity to both styles of cutting tasks can increase the complexity of the drill. If i'm structuring a session there are three ways I look to prescribe COD drills.
-
Planned COD (Max Quality)
-
Planned COD (Metabolic Focus)
-
Reactive COD (Max Quality)
Plyometric Focus
When it comes to progressing plyometrics from low amplitude and eccentric absorption progressions, focus shifts towards increasing the amplitude of jumps and hops, decreasing ground contact times and integration of lateral and rotational plyometrics.
Simple vector plyometrics are best utilised for improving rate of force development whilst more complex variations such as lateral and rotational options are best for exposing the athlete to increased proprioceptive demands.
The use of a double contact between a continuous jump / hop can be a useful stepping stone in order to dissipate the pressure that comes from each land and allow the athlete to re-organise themselves prior to the next hop.
Importantly, as running demands begin to increase; adequately prescribing more intensive plyos is critical in active load management for the athlete. I typically try to leave one session per week dedicated to intensive plyometrics (Jump Integration & beyond).
Performance Profiling
In addition to the aforementioned profiling battery listed above in the load introduction phase. Emphasis shifts towards measures of reactive strength index and thus the main additions into my testing battery include:
-
Triple Hop
-
Triple Crossover Hop
-
Timed 40/30 Lateral Hop
-
Drop Jump
-
Single Leg Drop Jump
When it comes to benchmarking for these tests, a reasonable starting place is to aim for 90% limb symmetry index on all single leg tests whilst I additionally set the following targets:
Single Leg Hop:
Males >80% the athletes height
Females >70% the athletes height
Timed 40/30
Males >50 hops in 30 seconds
Females >45 hops in 30 seconds
Drop Jump RSI
Males > 2.5
Females >2
Single Leg Drop Jump RSI
Males >1.5
Females >1.25
Training Integration & Return to Performance Phase:

Once an athlete reaches the training integration phase, majority of the cogs should be in place when it comes to their physical preparation training in the gym and on the field. In this stage of rehabilitation, the focus and key communication with coaching staff should be around an athletes return to skill exposure, contact and transitioning back to match play.

When it comes to return to contact for athletes, the design of specific drills needs to be individual to an athletes sport in order to yield the greatest gains from a physical and psychological perspective. With this considered, I like to break my drill design down by intensity and position that the athlete is going to be in and then design different categories based upon the athletes sport. Above is an example of a 6 stage return to contact continuum that can be integrated in an athletes session.
Role of PROMs
An under utilised component of assessment in athlete recovery is the utilisation of PROMs throughout a rehab journey. When it comes to knee rehabilitation, I believe a simple IKDC is easy to use and will give the practitioner an insight into the athletes knee health during ADLs
Conclusion:
The utilisation of a systems based approach allows a practitioner to be objective, stepped and planned with each stage of an athletes recovery. High grade MCL tears can represent a difficult rehabilitation in the amateur and semi professional space as there are many boxes that need to be ticked both clinically and athletically to ensure an athlete experiences a successful return to performance. Consideration of the mechanism of injury, and the anatomy of the MCL is important to early stage programming, whilst knowledge of integrated athlete programming can help to ensure optimal physical preparation. The above journey is a very non exhaustive list of options in regards to training drills, athlete planning and performance profiling, each athlete must be treated as an individual however I hope there are some takeaways that can be implemented in daily practice. At the very least I hope this blog has gotten you thinking about how your planning process works in the rehabilitation of sporting injuries.
Justin Richardson
www.sportsrehab.physio
www.athletesauthority.com.au
References:
Phisitkul, P., James, S. L., Wolf, B. R., & Amendola, A. (2006). MCL injuries of the knee: current concepts review. The Iowa orthopaedic journal, 26, 77–90.
Vosoughi, F., Rezaei Dogahe, R., Nuri, A., Ayati Firoozabadi, M., & Mortazavi, J. (2021). Medial Collateral Ligament Injury of the Knee: A Review on Current Concept and Management. The archives of bone and joint surgery, 9(3), 255–262. https://doi.org/10.22038/abjs.2021.48458.2401
Dambros, C., Martimbianco, A. L., Polachini, L. O., Lahoz, G. L., Chamlian, T. R., & Cohen, M. (2012). Effectiveness of cryotherapy after anterior cruciate ligament reconstruction. Acta ortopedica brasileira, 20(5), 285–290. https://doi.org/10.1590/S1413-78522012000500008
Rice DA, McNair PJ. Quadriceps arthrogenic muscle inhibition: neural mechanisms and treatment perspectives. Semin Arthritis Rheum. 2010 Dec;40(3):250-66. doi: 10.1016/j.semarthrit.2009.10.001. Epub 2009 Dec 2. PMID: 19954822.
Sebastian Bohm, Falk Mersmann, Alessandro Santuz, Arno Schroll, Adamantios Arampatzis (2021) Muscle-specific economy of force generation and efficiency of work production during human running eLife 10:e67182 https://doi.org/10.7554/eLife.67182
Kotsifaki A, Van Rossom S, Whiteley R, et al
Single leg vertical jump performance identifies knee function deficits at return to sport after ACL reconstruction in male athletes
British Journal of Sports Medicine 2022;56:490-498.
Kotsifaki, A., Korakakis, V., Graham-Smith, P., Sideris, V., & Whiteley, R. (2021). Vertical and Horizontal Hop Performance: Contributions of the Hip, Knee, and Ankle. Sports health, 13(2), 128–135. https://doi.org/10.1177/1941738120976363
Juneja, P., & Hubbard, J. B. (2022). Anatomy, Bony Pelvis and Lower Limb, Knee Medial Collateral Ligament. In StatPearls. StatPearls Publishing.
Endurance sport is one of the greatest tests of mental and physical toughness. During a marathon an athlete, on average, will complete 160-200 steps per minute. Whilst running has numerous benefits for our health and wellbeing, it can be monotonous loading on the skeletal system. Bony stress injuries account for up to 20% of running related injuries per year. It is believed that one reason for this is the repetitive overloading on runners’ bones. In comparison, activities involving irregular movements seem to foster greater bone health. The ultimate goal should always be injury prevention, so, should runners incorporate directional movements into their training repertoire for bone health?
Bone is an alive, adaptable, and dynamic structure. Our bone density increases as we grow and by 30 our density is at its peak. After this age we can only maintain what we have. Bone health refers to our bones’ mineral density and quality and is the result of a plethora of factors. In otherwise healthy runners, energy availability, biomechanics, training load and recovery, all play important roles in creating good bone health. Poor bone health can increase the risk of fractures during one’s developmental years and later in life.
There are two main theories that address the way in which our bones are loaded during running. The muscle-bone unit theory refers to the pulling forces created by a muscular contraction. The other references the ground reaction forces through bone when the foot contacts the ground, producing torsional and compressive load. Both mechanisms create macro-trauma which stimulates tissue production and shapes bones geometric structure. However, like other tissues in the body, the activity needs to be progressive otherwise the bone may become accustom and stop adapting. These principles may be used to help runners who may otherwise be stunting adaptation through habitual running load.
In general runners’ bones are healthier than sedentary people. Unfortunately, runners consistently demonstrate lower bone mineral density (BMD) when compared to matched individuals who partake in high impact and irregular movement based sports. A summary of the research of athletes (aged 14-30) found soccer, basketball and volleyball players as well as gymnasts, all displayed greater BMD than those who only ran. A study of young soccer players demonstrated that female players had healthier tibiae than runners and both genders had better density at the spine, femur and calcaneus. In separate studies of track athletes and infantry recruits those who also regularly participated in basketball had up to an 82% reduction in stress fracture risk. Interestingly, in masters athletes those who participated in sprinting had greater BMD than their peers who competed in long distance running. The benefits of diverse loading in youth were also found to protect runners later in life with some up to 50% less likely to sustain a stress fracture.
What seems to be more unclear is the ideal dosage for bony loading. Bone regeneration cycles are suggested to take 3-8months. Studies of humans, mice and turkeys found significant changes after as little as 3 weeks of a jump program. Repetition amount also widely varied between studies from 30 - 350 cycles per week. A study of adolescent females found that a 9-month plyometric program improved only greater trochanter bone strength. Another found plyometric training only benefited those who participated in low osteogenic sports such as swimming. Studies on structure found that rate, magnitude and activity resulted in site specific changes, however, no optimal values for load were presented. No well-known study was found to investigate an irregular, directional and high impact, loading program for the reduction of fracture risk in endurance runners.
It is important to note there are many other factors which influence bone health that have not been explored here. The body needs a plentiful supply of vitamin D and Calcium to build strong bone. To create an optimal environment for this rest and good sleep are also essential. For distance runners who are constantly in a state of low energy availability, bone loading has been found to have little strengthening effects and can be somewhat detrimental if added in addition to their normal training.
Runners want to run. Convincing them to do otherwise continues to remain a great challenge for clinicians, however, it would seem that some variety may strengthen their bones. Youth runners should be encouraged to participate in a variety of sports. Once specialisation occurs, a runner may benefit from incorporating direction and plyometric loading into their training. Unfortunately, the optimal dosage for this is largely unknown.
References
Beck, B. R., Daly, R. M., Singh, M. A. F., & Taaffe, D. R. (2017). Exercise and Sports Science Australia (ESSA) position statement on exercise prescription for the prevention and management of osteoporosis. Journal of Science and Medicine in Sport, 20(5), 438-445.
Gómez Bruton, A., Matute-Llorente, Á., González-Agüero, A., Casajus, J., & Vicente-Rodríguez, G. (2017). Plyometric exercise and bone health in children and adolescents: a systematic review.
Gómez-Cabello, A., Ara, I., González-Agüero, A., Casajús, J. A., & Vicente-Rodríguez, G. (2012). Effects of training on bone mass in older adults: a systematic review. Sports Med, 42(4), 301-325.
Hart, N. H., Nimphius, S., Rantalainen, T., Ireland, A., Siafarikas, A., & Newton, R. U. (2017). Mechanical basis of bone strength: influence of bone material, bone structure and muscle action. Journal of musculoskeletal & neuronal interactions, 17(3), 114-139.
Hong, A. R., & Kim, S. W. (2018). Effects of Resistance Exercise on Bone Health. Endocrinology and metabolism (Seoul, Korea), 33(4), 435-444. doi:10.3803/EnM.2018.33.4.435
Kato, T., Terashima, T., Yamashita, T., Hatanaka, Y., Honda, A., & Umemura, Y. (2006). Effect of low-repetition jump training on bone mineral density in young women. Journal of Applied Physiology, 100(3), 839-843.
Nattiv, A. (2000). Stress fractures and bone health in track and field athletes. J Sci Med Sport, 3(3), 268-279.
Scofield, K. L., & Hecht, S. (2012). Bone health in endurance athletes: runners, cyclists, and swimmers. Curr Sports Med Rep, 11(6), 328-334.
Tenforde, A. S., & Fredericson, M. (2011). Influence of sports participation on bone health in the young athlete: a review of the literature. Pm r, 3(9), 861-867.
Tenforde, A. S., Sainani, K. L., Carter Sayres, L., Milgrom, C., & Fredericson, M. (2015). Participation in ball sports may represent a prehabilitation strategy to prevent future stress fractures and promote bone health in young athletes. Pm r, 7(2), 222-225.
Vlachopoulos, D., Barker, A. R., Ubago-Guisado, E., Williams, C. A., & Gracia-Marco, L. (2018). The effect of a high-impact jumping intervention on bone mass, bone stiffness and fitness parameters in adolescent athletes. Archives of osteoporosis, 13(1), 128-128.
Witzke, K., & Snow, C. (2000). Effects of plyometric jump training on bone mass in adolescent girls. Medicine and science in sports and exercise, 32, 1051-1057.
Wright, A. A., Taylor, J. B., Ford, K. R., Siska, L., & Smoliga, J. M. (2015). Risk factors associated with lower extremity stress fractures in runners: a systematic review with meta-analysis. British Journal of Sports Medicine, 49(23), 1517.
T-Junction injuries of the distal biceps femoris – a more severe variant of hamstring strain injury
Although there are signs of a drop in the number recurrences of hamstring strain injuries (HSIs) in sport[1], it has been long evident both epidemiologically and experientially that these are amongst the most challenging in sport. In fact, since re-injuries have been reported to occur in up to 63% of HSIs[2], it is obvious that it is this recurrence risk underpins the high rates of HSI in sport. If these recurrences could be reduced, it would have an exponential effect on reducing the burden of this injury. What’s more, as these reinjuries typically present having worsened radiologically, they have a significant effect on a club’s injury burden [3].
An important development thus, has been the evolution in imaging classifications that have allowed for bespoke diagnosis, management and rehabilitation. These are particularly important in professional sport where rapid access to MRI common, to meet the pressurized demands of competition and contracts. The widespread adoption of classification systems such as the British Athletics Muscle Injury Classification (BAMIC)[4] mean that modern sports medicine now gives consideration to anatomical location in addition to grading, and can modify expectations accordingly. Although the research so far has been mixed [5, 6], some studies have demonstrated prolonged time to return to play and increased recurrence risk following intramuscular tendon injury in athletes [7-10].
This development has now widely expanded the considerations for clinicians in rehabilitation. Macdonald, McAleer [11] have described a tailored exercise progression with consideration of load, speed and contraction type dependant on BAMIC classification, while Askling, Tengvar [12] has discussed the variation in outcome following stretch and sprint type HSI. Hence, it’s now clear that all HSIs should not be thought to be the same, and they should not be homogenised from a prognostic or management perspective. In order to best mitigate against recurrence, it is necessary to understand the characteristics of each sub-type.
The most frequently injured of the hamstring muscles is the biceps femoris (BF) in running sports [13-15]. While these typically occur at the proximal musculotendinous junction (MTJ), a single retrospective analysis by a Super 15 rugby union team noted higher incidence of distal injuries than had otherwise been previously been reported [14]. Huygaerts, Cos [16] have extensively reviewed the anatomical and morphological features of BF that may predispose it to greater injury risk. As it’s name suggests, BF has two heads – the biarticular long head (LH) forming a conjoint tendon with semitendinosus proximally, and a second monoarticular short head (SH) which functions primarily as a knee flexor. These heads are innervated separately by the common peroneal and tibial nerves respectively.
Importantly, Entwisle, Ling [13] has recently descripted the distal MTJ ‘T-Junction’ of the biceps femoris, formed by a complex confluence of the epimyseal surface of the LH and SH in the distal posterior thigh (Image 1). Injuries to this location have been suggested to be a more severe variant of HSI that should, like intramuscular tendon injuries, be treated as a distinct clinical entity [13, 17].
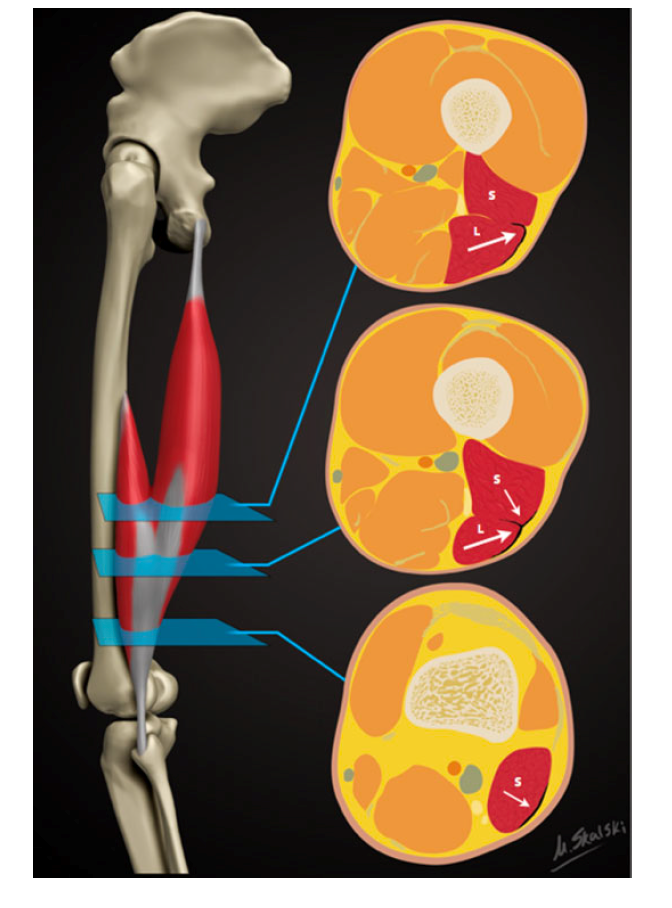
Figure 1: Reproduced from Entwisle, Ling [13]. A schematic demonstrating the sequential axial anatomy of the T junction of the biceps femoris distal musculotendinous junction (MTJ). Proximally, the anterolateral epimyseal surface of the long head (L) condenses to form the proximal portion of the distal MTJ and appears L-, C-, or U-shaped. In the midportion, the opposing epimyseal condensations as the anterolateral aspect of the long head and posterolateral aspect of the short head (S, small arrow) form the DMTJ that appears as a T-shaped structure. Distally, the posterolateral epimyseal condensation of the short head forms the DMTJ and appears as a shallow convex structure.
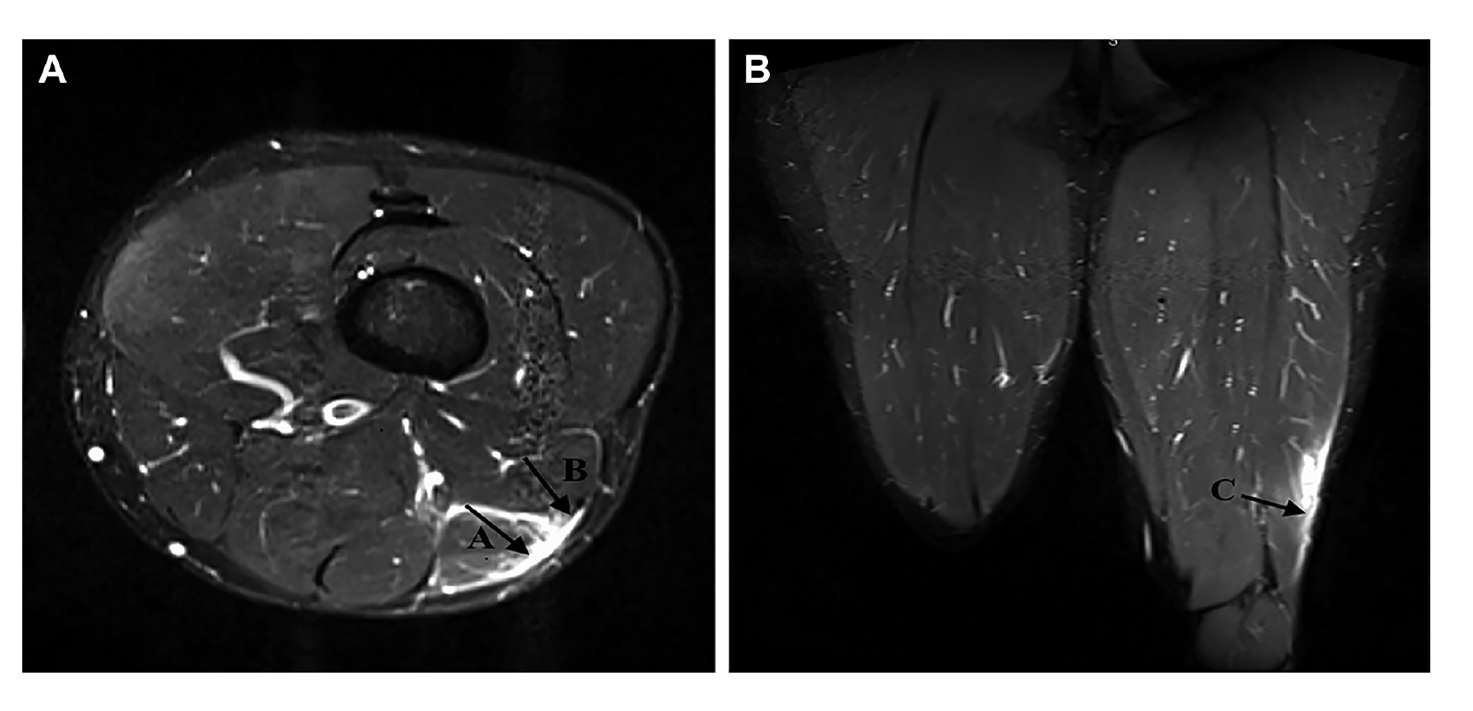
Figure 2: Reproduced from Kayani, Ayuob [17]. Axial section T2-weighted MRI slices showing grade 3 injury to the distal musculotendinous T junction of the biceps femoris with surrounding peritendinous oedema.
Presently, however, there is a vacuum of information to guide us. Firstly, no characteristic mechanism of injury has been described that is associated with T Junction strain. While semimembranosus and proximal free tendon injuries have been shown to occur during overstretch, there is no distinct pattern of T Junction injury. Table 1 outlines the mechanisms of injury of a small subset of athletes who incurred a T Junction injury, but this is by no means an exhaustive analysis of the biomechanical factors involved. Some muscle injury classification systems have been proposed that include the mechanism of injury[18], and these would add value in this case in rising suspicion of such an injury that can only be determined using imaging. With further longitudinal analysis to better understand injury mechanism, preventative strategies – via exercise selection and skill execution – could be designed and trialled.
In addition, no study has described the clinical characteristics of such injuries. There are no proven pathognomic signs that should alert the clinician to the suspected presence of an injury in this location, other than palpation around the distal MTJ. So far, as these injuries can only be identified using MRI and thus, they are most frequently detected in elite sports people. In fact, it is suspected that in many cases these are never identified. This may result in frequent recurrences of BF strains over prolonged periods of time in sub-elite athlete athletes. It has been reported that these injuries become ‘relatively symptom free’ 3-4 weeks following injury, which may lull clinicians into under-estimating the prognosis of such an injury and progressing too rapidly through the return to play process
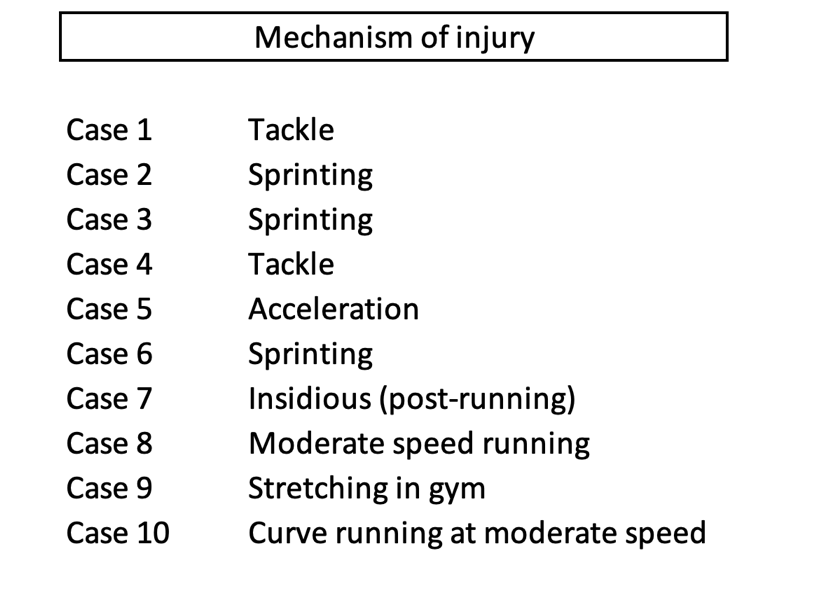
Table 1: Brief description of mechanism of T-Junction injuries observed in 10 cases in a cohort of rugby union players
This early resolution of symptoms may cause the frequency of early recurrences that has been described for this sub-type, with 76% of recurrences occurring within the first 3 months [13]. Incomplete aponeurotic healing remains at 6 weeks following injury [19], so perhaps one principle of management would be a more cautious approach with consideration of the stages of healing.
Periodisation of rehabilitation should give consideration to three keystones – (1) anatomical diagnosis, (2) functional diagnosis or limitations and (3) the demands of ‘return to sport’. Given the nature of the anatomical diagnosis in this case, and the risk of early recurrence, it is proposed that a gentler cadence through the process is best. As with the recommendations for intramuscular tendon injury [11], sprinting activities and exercises involving maximal length, high force and rate of loading should be programmed in a manner that respect immature histological healing at the location of injury.
Consideration should also be given to the distinct characteristics of the distal BF that could be implicated in the poor recovery from injuries in this location as identification of these directs the strength training interventions[20]. The proximal and middle regions of the BFlh have larger pennation angles and greater fascicle lengths than the distal portion [16]. Although this has not prevented the proximal hamstring from being more frequently injured, perhaps the shorter fascicle lengths of the distal hamstring are implicated in poor recovery when injury does occur. Similarly, the distribution of fibre types is not uniform throughout the muscle, with a greater proportion of type 2 muscle fibres existing proximally. This could impact upon the type of training that is deemed optimal for this region.
The duel innervation of the BF is consistently suggested as a potential reason for the high proportion of injuries to this muscle. Given T-junction injuries occur at the confluence of the two heads, it is logical that an asynchrony in co-ordination of the heads could contribute. However, how this can be quantified, and resolved, is unclear and it is only speculative as to what approach could be taken. Macdonald, McAleer [11] suggest isometric exercises as a tool to overcome the neuromuscular inhibition that exists during eccentric exercise following injury[21], and a similar approach may yield benefit in injuries at this confluence.
Recent research has demonstrated the differences in inter-muscular activation during various exercises [20], and has allowed for increasing specificity in rehabilitation. The ‘Nordic hamstring exercise’ and ‘single-leg hip extension’ elicit high activity in the biceps femoris muscle, and thus exercises with these characteristics should be considered important for eliciting an adaptation, while also treated with caution given they are likely to stress this area. Subsequently, Hegyi, Csala [22] has expanded upon this, by demonstrating region specific differences within individual muscles (Figure 3). The eccentric component of the straight knee bridge, upright hip extension conic-pulley and slide leg curl may be most appropriate if attempting to elicit a location specific response in this region, with contraction type adapted dependant on whether the goal is to overcome inhibition (isometric), develop fascicle length or local strength and hypertrophy (eccentric), or simply to induce healing through mechanotherapy. However, again, it is not known whether these injuries occur due to compensation for proximal dysfunction – at which point offloading distally would be the targeted outcome. In the absence of this information, a balanced programme is advised, giving cognisance to inter-muscular and proximal-distal biases, across multiple contraction types.
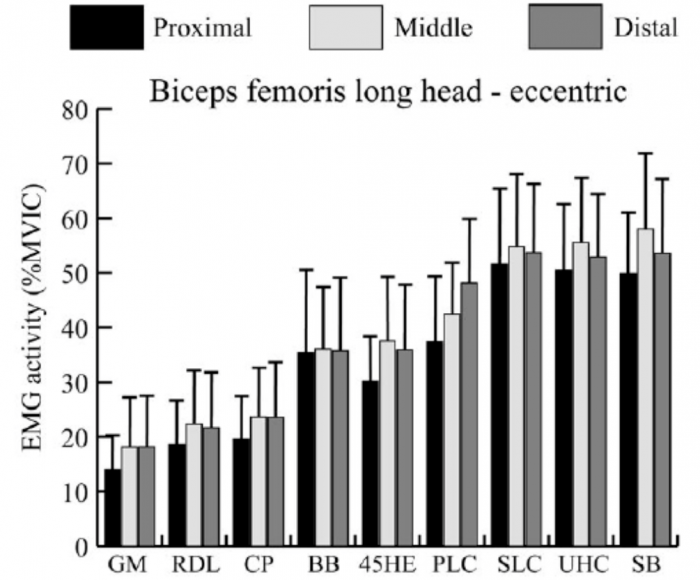
Figure 3: Reproduced from Hegyi, Csala [22]. Mean and standard deviation of the normalized activity level (%MVIC, maximal voluntary isometric contraction) in the proximal, middle, and distal regions of each muscle during the eccentric phase of each exercise. GM, good morning; RDL, unilateral Romanian deadlift; CP, cable pendulum; BB, bent‐knee bridge; 45HE, 45 degree hip extension; PLC, prone leg curl; SLC, slide leg curl; UHC, upright hip extension conic‐pulley; SB, straight‐knee bridge
Given that early recurrence is a key feature is this injury, the pace of progression is critical. If attempting to offload the distal BF, exercises that preferentially activate the medial hamstring or proximal BF may be indicated. In addition, initially restricting range of motion and rate of force development, as well as muscle length across the two involved joints are characteristics of exercise selections that can be manipulated and progressed, while still giving consideration to prioritising the adaptations that might be necessary to prevent recurrence (Table 4).
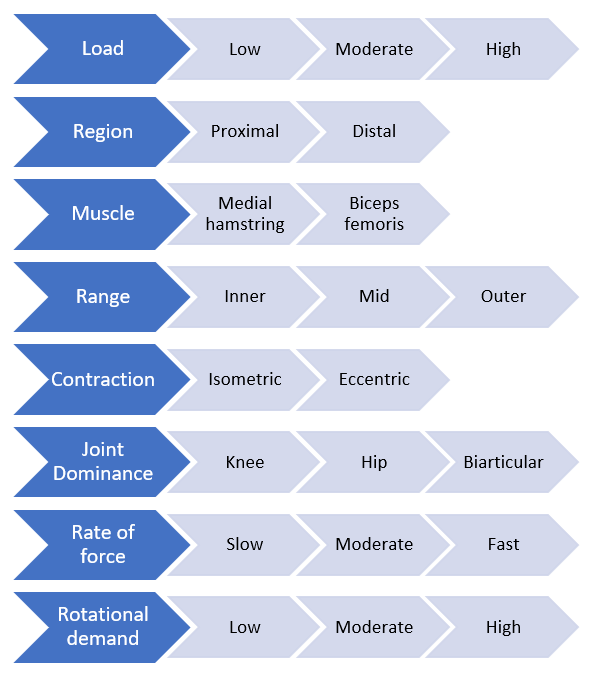
Figure 4: Proposed conceptual progressive loading model specific to a hamstring strain injury
In conclusion, it’s clear that an even more complete approach to rehabilitation is required following T-Junction than for a typical HSI, giving consideration to the structural diagnosis and characteristics of the distal BF. At present however, it remains unclear which anatomical and morphological traits have the greatest influence on injury risk, nor which approaches will generate the most specific and appropriate adaptation. In addition, strategies that help with the identification of these injuries and raise suspicion amongst clinicians would likely improve management of this complex variant of HSI.
References:
- Ekstrand, J., et al., Injury rates decreased in men's professional football: an 18-year prospective cohort study of almost 12 000 injuries sustained during 1.8 million hours of play. Br J Sports Med, 2021.
- de Visser, H.M., et al., Risk factors of recurrent hamstring injuries: a systematic review. Br J Sports Med, 2012. 46(2): p. 124-30.
- Koulouris, G., et al., Magnetic resonance imaging parameters for assessing risk of recurrent hamstring injuries in elite athletes. Am J Sports Med, 2007. 35(9): p. 1500-6.
- Pollock, N., et al., British athletics muscle injury classification: a new grading system. Br J Sports Med, 2014. 48(18): p. 1347-51.
- van der Made, A.D., et al., Intramuscular tendon involvement on MRI has limited value for predicting time to return to play following acute hamstring injury. 2018(1473-0480 (Electronic)).
- van der Made, A.D., et al., Intramuscular tendon injury is not associated with an increased hamstring reinjury rate within 12 months after return to play. 2018(1473-0480 (Electronic)).
- Pollock, N., et al., Time to return to full training is delayed and recurrence rate is higher in intratendinous ('c') acute hamstring injury in elite track and field athletes: clinical application of the British Athletics Muscle Injury Classification. Br J Sports Med, 2016. 50(5): p. 305-10.
- Eggleston, L., M. McMeniman, and C. Engstrom, High-grade intramuscular tendon disruption in acute hamstring injury and return to play in Australian Football players. Scand J Med Sci Sports, 2020.
- Comin, J., et al., Return to competitive play after hamstring injuries involving disruption of the central tendon. Am J Sports Med, 2013. 41(1): p. 111-5.
- Vermeulen, R., et al., Complete resolution of a hamstring intramuscular tendon injury on MRI is not necessary for a clinically successful return to play. Br J Sports Med, 2020.
- Macdonald, B., et al., Hamstring rehabilitation in elite track and field athletes: applying the British Athletics Muscle Injury Classification in clinical practice. Br J Sports Med, 2019. 53(23): p. 1464-1473.
- Askling, C.M., et al., Proximal hamstring strains of stretching type in different sports: injury situations, clinical and magnetic resonance imaging characteristics, and return to sport. Am J Sports Med, 2008. 36(9): p. 1799-804.
- Entwisle, T., et al., Distal Musculotendinous T Junction Injuries of the Biceps Femoris: An MRI Case Review. Orthop J Sports Med, 2017. 5(7): p. 2325967117714998.
- Kenneally-Dabrowski, C., et al., A retrospective analysis of hamstring injuries in elite rugby athletes: More severe injuries are likely to occur at the distal myofascial junction. Phys Ther Sport, 2019. 38: p. 192-198.
- Askling, C.M., et al., Acute first-time hamstring strains during high-speed running: a longitudinal study including clinical and magnetic resonance imaging findings. Am J Sports Med, 2007. 35(2): p. 197-206.
- Huygaerts, S., et al., Does Muscle-Tendon Unit Structure Predispose to Hamstring Strain Injury During Running? A Critical Review. Sports Med, 2021. 51(2): p. 215-224.
- Kayani, B., et al., Surgical Repair of Distal Musculotendinous T Junction Injuries of the Biceps Femoris. Am J Sports Med, 2020. 48(10): p. 2456-2464.
- Valle, X., et al., The MLG-R muscle injury classification for hamstrings. Examples and guidelines for its use. Apunts. Medicina de l'Esport, 2019. 54(202): p. 73-79.
- Jaspers, R.T., et al., Healing of the aponeurosis during recovery from aponeurotomy: Morphological and histological adaptation and related changes in mechanical properties. Journal of Orthopaedic Research, 2005. 23(2): p. 266-273.
- Bourne, M.N., et al., An Evidence-Based Framework for Strengthening Exercises to Prevent Hamstring Injury. Sports Med, 2018. 48(2): p. 251-267.
- Fyfe, J.J., et al., The role of neuromuscular inhibition in hamstring strain injury recurrence. J Electromyogr Kinesiol, 2013. 23(3): p. 523-30.
- Hegyi, A., et al., High-density electromyography activity in various hamstring exercises. Scand J Med Sci Sports, 2019. 29(1): p. 34-43.
- Hegyi, A., et al., Individual Region- and Muscle-specific Hamstring Activity at Different Running Speeds. Med Sci Sports Exerc, 2019. 51(11): p. 2274-2285.
The dream for many sportspeople is to forge a long and successful career as a full-time professional athlete. However, only very few are lucky enough to experience this, and many more athletes across the world end up showcasing their talents as a part-time or semi-professional athlete.
Rather than having the luxury of dedicating most of their time to training and recovery, these athletes are required to work full time jobs (often labour intensive), and then attend training sessions at the end of a 10 hour work day, with training loads very similar to that of an elite athlete.
This obviously poses a massive challenge to the athlete. Having to try and fit in work, training, recovery, family time, social time and sleep all in the space of a 24 hour day.
Managing these athletes can also be a massive challenge for the sports physiotherapists helping them to rehabilitate their injuries and keeping them out on the park.
As we know, load management is an integral part of progressing through a rehabilitation plan, and also helping to reduce the risk of any niggles or injuries. Over the past few years, even with limited resources at semi professional sporting organisations, physios and S+C staff have become much better at monitoring and analysing player loads from a physical, mental and emotional perspective. However, this is where the real challenge lies in dealing with players who work physical jobs throughout the day. For example, take a player who has suffered a calf strain 10 days ago. We can’t expect a player to tell us exactly how many times he has gone up and down the ladder during his work day as an electrician, but should this be a consideration in how much running he does at training that night?
For the athlete playing at this level, at the end of the day, their paid work is a higher priority for the majority of them over their ability to play sport. This often means that rehabilitation from an injury is compromised or lengthened in time, due to the pressures of having to return to work and feed their families. Take the athlete who has had an ACL reconstruction, but also works as a carpenter. The athlete will be eager to return to full time work as soon as they get the all clear from their surgeon, but will being on their feet all day and repetitively squatting cause a knee effusion that will then hinder their ability to perform and progress their strength work?
As their sport might not be their number one priority in their lives as mentioned, training consistency can also be a challenge in dealing with players at this level. Work and family commitments can sometimes clash with training sessions, with missed training sessions affecting their training load for that week, and potentially increasing their risk of injury in the coming weeks.
The emotional toll that having to fit so much into one day can take on the athlete, is also a vital consideration as a sports physiotherapist at this level. We are in a great position as sports physiotherapists to chat to players to ask them how they are coping. Whilst strapping their ankle, we can gain a lot of information about whether or not the athlete has a rough day or period or time, and whether or not they should have a lighter night on the track to help not overload their nervous system.
Many challenges and questions have been posed above, but the number one question is what can we as sport physiotherapists do to help semi-professional athletes overcome these challenges?
In my opinion, the best thing we can do here is to educate our athletes as much as possible, and focus on the ‘big-ticket’ items to allow them to stay at their best for as long as possible.
The ‘big-ticket’ items for me are:
- Sleep – As we know, sleep has been shown to be the most important recovery technique out there for athletes. Sleep is available to both professional and semi-professional athletes, so this has to be a priority.
- Importance of communication – Empower and encourage the athletes to communicate with coaches, S+C staff and physios so we can better monitor how they are dealing with the challenges of being a semi-professional athlete.
- Training consistency – Missing a 10km training session during the week and not making up for it, can often lead to an injury down the track from my experience. It is up to the S+C coach, physio and athlete to formulate a plan as to how to best make up for this session.
I am sure for those sport physiotherapists out there who work at this level with athletes, these are common challenges for you, along with many more that I have not mentioned. Because of these challenges, I find working with these athletes highly enjoyable and rewarding, and I hope you do too!
Free access to Jarrod Wade's presentation on Rehabilitation for Match Demands
[spu popup="1088"]

- Hamish's thoughts on his experiences working as a head Physio in both professional rugby and the AFL
- What to expect from Hamish at the Upper Limb Rehabilitation in Sport course in the Gold Coast
- Posterior dislocation- what are the tell tale signs?
- Where early management is different between posterior & anterior dislocations
- Common imaging findings following both posterior & anterior shoulder dislocations
- Decision making around surgical Vs non surgical management following instability episodes (see further detailed notes below)
- Differences in post surgical management for anterior and posterior repairs
- Post surgical rehabilitation
- Early exercises & targets
- Time based expectations on restoring ROM and strength
- How & when to introduce pushing, pulling and over head
- How and when to take the athlete into venerable positions (Abd/ ER
- Testing or benchmarking in readiness for a return to play
- What is often missed in shoulder rehabilitation
- Contact based conditioning
- Occupation: overhead/manual labour vs sedentary
- Sporting demands – collision sports
- Co-morbidities/physical inactivity – prolongs recovery
- Evidence based surgical indications (reduces the chance of recurrence): Male <25 y/o with traumatic MOI, requires relocation + high functional demands = EBP supports surgical repair. Generally the risk factors from the literature for recurrent instability include: young age (<40 = 13x higher; majority occurring <25), being a male, contact sport. I would also include young females in collision sports in this category. However it is a discussion and as we discussed there is evidence that people in this group can have a positive outcome without surgery.
- Hypermobility:
- I always question the patient about their episode(s) – patients can use the words dislocation and subluxation synonymously. True dislocation or instability in the absence of dislocation. I always I always question the patient around the MOI and do they have imaging evidence of the dislocation (in ED)/needed someone to relocate the shoulder… If their story is accurate for the MOI then I generally believe them when they say their shoulder dislocated. If they haven’t had true dislocation, rather instability episodes – conservative treatment. Especially if you’re dealing with someone who has more mobility than the average (>4 Beighton’s).
- Traditional classification include the TUBS (Traumatic, unilateral, Bankart, Surgery) and AMBRI (Atraumatic, Multidirectional instability, Bilateral, Recurrent, Inferior Capsular Shift), however this 2nd population doesn’t do as well with surgery as was initially intended with this classification, so conservative path is the best here. A further classification system – The Stanmore Classification (diagram below) further stratifies it into 3 groups and the relationship between trauma, structure and muscle patterning – article attached. In short, group I relates to traumatic dislocation and structural failure, group II with structural laxity that can pre-dispose them to instability with or without trauma, group III to muscle patterning issues causing instability/resting subluxation. Surgery is indicated in group I and only considered in group II with structural failure and who have failed a good rehab program.
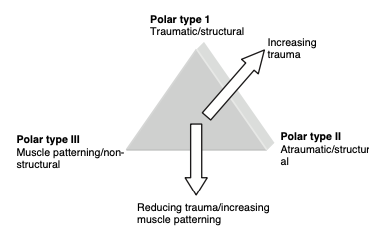 Reference article: Jaggi & Lanbert 2010, Rehabilitation for Shoulder Instability
Reference article: Jaggi & Lanbert 2010, Rehabilitation for Shoulder Instability
- Bone stress injuries
- The energy deficit athlete
- Prevention systems in endurance athletes
- Reducing the incidence of patella tendinopathy in volleyball athletes
- Groin injury prevention
- What to expect at the Athlete Groin Pain Symposium in Sydney
- Isometric hamstring strength assessment as a screening tool
- Ongoing isometric hamstring strength deficit following hamstring injury
- Who owns injury & performance?
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher. We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
This episode is brought to you by KangaTech & West Coast Health & High Performance (Perth)

- The current state of Sports Physiotherapy
- Tendinopathy
- Spraino & lateral ankle sprain prevention
- Hip ABDuctor & ADDuctor strength and it's relation to groin pain
- Adductor strengthening - why the adductors?
- The Copenhagen- How much is enough and is it sufficient for groin pain prevention?
- How should the groin terminology consensus be used to guide management?
- The HAGOS
- Return to Sport post Hip Arthroscopy
- What are the most important aspects of ACL prevention?
- How to facilitate an optimal learning environment at courses & conference
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
This episode is brought to you by KangaTech & West Coast Health & High Performance (Perth)

In this 13th Episode of The Sports MAP Podcast we chat with Chris Perkins about Athletic Lower Back Pain. Chris is s specialist sports Physiotherapist and has worked at the West Coast Eagles (AFL) for past 16 years. He has also worked extensively with world renowned back pain expert Peter O'Sullivan. In this episode we discuss:
- Chris's professional Journey
- The challenges of blending work in professional sport and running a private clinic
- Managing an athletic lower back pain presentation
- Subjective cues
- Objective assessment
- Common contributing factors and how to address these
- Managing work load
- Imaging & red flags
- The use of non threatening language & communication
- Gym based exercises and low back pain
- And more
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
This episode is brought to you by KangaTech & West Coast Health & High Performance (Perth)

In this 11th Episode of The Sports MAP Network Network we chat with previous Head Physiotherapist for the England Rugby League team Dave O'Sullivan around Syndesmosis Injury Rehabilitation & Dave's Return to Play Systems for lower limb Injury.
- Early focus area's in rehabilitation of a Syndesmosis injury
- Strength assessment & criteria
- Dynamic calf assessment
- Lunge progressions & the importance of the peroneas tertius
- Hopping progressions
- Agility /offline progressions
- Troubleshooting
- Return to running prescription
- Return to play
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
This is episode is brought to you by Archies Footwear
Archies are offering all listeners of our podcast a 20% discount on any order (big or small). Simply use the code Sports_MAP when ordering from www.archiesfootwear.com

Welcome to the 10th Episode of the Sports MAP Podcast.
In this Episode we chat to St Kilda Football Club (AFL) Physiotherapist and director of the Hip & Groin Pain Clinic Andrew Wallis on the key aspects in the assessment, diagnosis and management of Hip Dysplasia including:
- What actually is Hip Dysplasia
- How Andrew developed an interest in Hip Dysplasia
- Subjective clues in assessment and key questions to ask patients
- Key objective findings to assist in making a clear diagnosis
- The importance of differentiating FAI and Hip dysplasia
- Pain drivers in hip dysplasia
- Imaging and radiological findings
- Management options available
- Setting expectations
- Conservative management and rehabilitation guidelines
- Return to running and sport
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
This is episode is brought to you by IMeasureU and Vald Performance

/
In this Episode #7 of the Sports MAP Podcast we chat with Enda King around his approach to the Rehabilitation of Complex Athletic Groin Pain using a case example.
- Determining if this athlete is suitable for Rehabilitation
- Assessment protocols
- Addressing & identifying movement based impairments
- Assessment of speed & power in Athletic Groin Pain
- Imaging & the significance of bone marrow edema
- Diagnosis and the entity based approach
- Rehabilitation strength measures
- Return to running & change of direction
- Return to Sport
- Key influences in Enda' career
- And more
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
This is episode is brought to you by IMeasureU and Vald Performance
Show Notes/ References
Clinical & Biomechanical outcomes of Rehabilitation targeting intersegmental control
Enda King Groin Rehabilitation Video Series