
In this episode of the How I Rehab podcast by Sports MAP we chat with Performance and Rehab manager at New England Patriots, Emidio Pacecca.
Emidio has extensive experience working in elite sporting environments including the Carlton Blues in the AFL, the Australian Institute of Sport (AIS) and Western Force Rugby Union team.
In this episode we cover a range of topics including:
- Emidio’s experience and journey to get to the NFL
- Expectations and responsibilities within an NFL team
- Early strategies around Achilles tendon injuries within the NFL
- Loading protocols
- Isometric loading expectations
- High speed running dosage and hamstring loading
- Strength training expectations across different sports
- Quantifying strength levels
Listen to this Podcast via your favourite platform including Apple, Spotify, Player FM & Stitcher.
You can also VIEW this Podcast on the Sports MAP YouTube channel.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook

In this 30th episode of the Sports MAP Podcast we chat with co-founder and Head Physiotherapist for Rehab 4 Performance in Liverpool, Matt Konopinski. Matt is a highly decorated specialist sports physiotherapist practicing in the UK.
Matt has over 15 years of experience working at the highest level of professional football. He has worked as the Head Physiotherapist for Liverpool, Rangers and Barnsley FC. Additionally, Matt has spent time as Men’s team Physiotherapist at the FA, England’s football governing body. He specialises in lower limb rehabilitation and optimising performance through biomechanics.
In this episode we cover a range of topics including:
- Matt's background in elite men's football, Liverpool FC
- Matt's interest and experience in knee injury rehabilitation
- Importance of recognition and optimal management of LCL injuries
- Mechanism of the injury
- LCL injuries in conjunction with additional knee injuries
- Assessment and diagnosis stategies
- Imaging
- Surgical vs non-surgical
- Bracing processes
- Key strengthening
- Return to run
- Return to kicking progressions
Listen to this Podcast via your favourite platform including Apple, Spotify, Player FM & Stitcher.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook

In this 29th episode of the Sports MAP Podcast we chat with Lead Physiotherapist of the Matildas, Australian Womens Football Team, Jaclyn Benz. Jaclyn has immense experience working at all levels of womens football. Her experience extends well beyond Women's Football after spending timeworking as a Locum at the Australian Institute of Sport and Hunter Sports Academy.
In this episode we cover a range of topics including:
- Jaclyn's background and pathway to her current position
- Her day-to-day experience of the recent World Cup
- Training and prep for the World Cup campaign
- Individualising injury prevention programs
- Injury differences between womens and mens sport
- Challenges and opportunities within womens elite football
- Management of Sam Kerr's calf injury
- Pressures and celebrations throughout the World Cup campaign
Listen to this Podcast via your favourite platform including Apple, Spotify, Player FM & Stitcher.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook
As you know, you should begin high-quality rehabilitation immediately after an injury. Everyone with an acute knee injury (e.g. ACL rupture, MCL injury, meniscal tear…) experiences early loss in muscle mass and muscle strength. So the first phase is crucial!
Overuse injuries also require adequate load management to reduce pain and increase load capacity.
Can we reduce these losses and restore them more early with Blood Flow Restriction Training (BFRT)? Can we reduce pain with BFRT?
Yes you heard that right! Blood Flow Restriction Training is able to increase muscle mass and strength with much less weights or NO weights at all. Which is absolutely important to maintain and improve post knee injury to restore daily functioning and participation to sports!
Experts Agree on the Recommendation to Use BFR in ACL Rehab
(Practice guideline Kotsifaki et al., 2023)
Based on the scientific evidence, high intensity strength training is necessary to get these improvements. But all of you know that training with heavy loads is far from possible after an acute knee injury. We need to protect tissue healing and respect the reduced load capacity of the knee! Especially when there are weight bearing restrictions given by the surgeon because of for example a meniscal repair.
So we have no other choice than applying low intensity training in these cases. But almost always muscles aren’t getting into fatigue and thus you aren’t experiencing the feeling of the pump, because of the very high amount of repetitions needed. The pump is actually very important to achieve because we then know that mechanisms are taking place and we are reducing the loss or even gaining muscle mass and strength.
Typically with overuse injuries, patients or athletes experience pain and are unable to tolerate the loading that occurs during training or high intensity strength exercises. Current research is suggesting that BFRT could reduce knee pain (e.g. anterior knee pain, patella femoral pain, patellar tendinopathy). This isn’t the only advantage of BFRT. Imagine your patient or athlete is already able to experience the physiological benefits associated with training at a higher intensity, meaning they are already building muscle mass and strength, or at least maintaining them without performing high intensity strength training.
Researchers found that BFRT can improve cross-sectional area and stiffness of the patellar tendon in healthy individuals. This is interesting to consider regarding the rehab of patellar tendinopathies, but should be further investigated!
BFR is no Magic! It's Pure Exercise Physiology
#CHASETHEPUMP
Besides that, BFR could:
- Reduce loss in bone mineral density and bone mass
- Possibly reduce swelling
- Possibly resolve activation problems
- Maintain or improve aerobic capacity, muscle mass and muscle strength with Aerobic BFRT
- Improve physical functioning and quality of life
- Be used safe in adolescents
LL-BFR Outperforms LL Training without BFR
How should BFRT be applied?
Step 1: is there an indication?
Who is likely an appropriate BFR training candidate? The evidence strongly supports BFR’s use in those patients with either a loading problem or a pain problem.
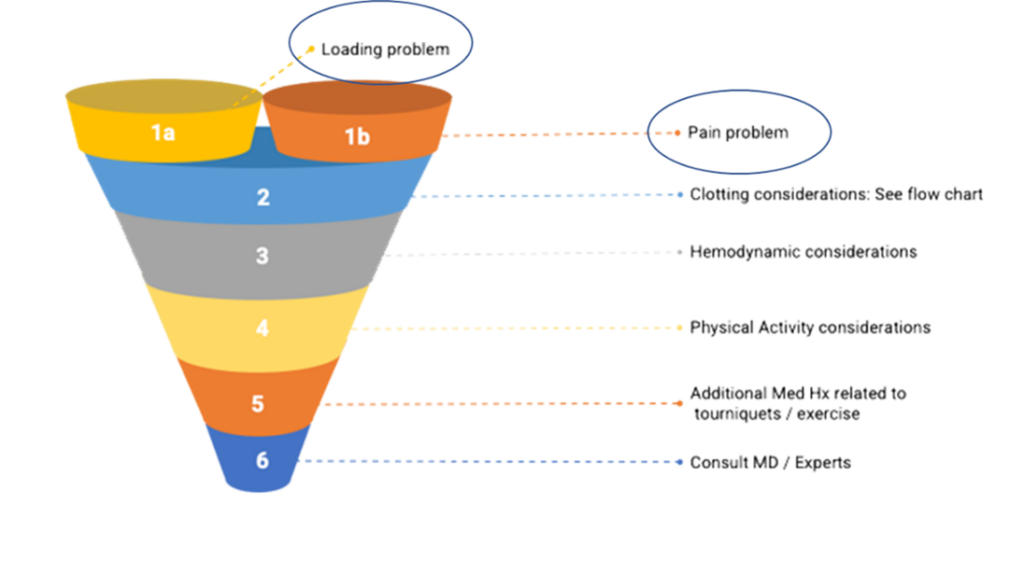
There is no discussion that there is an indication after for example ACLR or other serious knee injuries. Because load capacity is suppressed and pain is a major factor influencing the knee function.
Step 2: is it safe?
The evidence does not support the assertion that BFR creates blood clots! It seems to reduce the possibility of a blood clot.
BFR is safe if the following requirements are met:
- Medical screening passed
- Rule out absolute contra-indications
- Take into account relative contra-indications
- Blood pressure assessment
- Consult with doctor or expert (when in doubt)
- Applied by an experienced and trained therapist
- Correct protocols and techniques applied
- Use of objective LOP (limb occlusion pressure) assessment and pneumatic cuffs or validated automatic devices
- DON’T USE STRAPS
- DON’T USE PRESSURE BASED ON LEG CIRCUMFERENCE SOLELY
- Choose your cuffs wisely!

Stop Guessing! Start Assessing!
Step 3: write a BFR training program!
Writing a BFR training program includes taking into account medical screening and patient characteristics. Determining the training pressure based on a LOP assessment and prescribing based on the pressure/load continuum are crucial! When necessary, implement strategies to reduce perceptual demands to maintain long-term compliance. Last but not least, think about The Pillars of BFR Training throughout your training and within each session. Use them as a progressive framework/ continuum to applying BFRT from very easy to harder and select the right exercises.
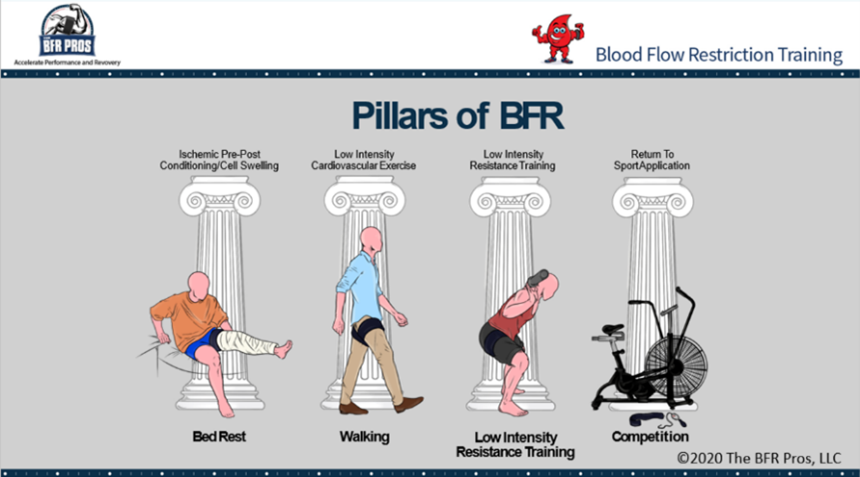
Pillar 1: cell swelling/ passive BFR
Goals of Pillar 1:
- Short familiarization period
- Reduction in atrophy and muscle strength loss
Pillar 2: cardiovascular training
Goals of Pillar 2:
- Increase in muscle mass and strength
- Maintenance or improvement of aerobic capacity
- Pain relief
- Bridge towards pillar 3
Pillar 3: resistance training
Goals of Pillar 3:
- Pursue the same benefits as with traditional high load strength training without all the external mechanical stress
- Attenuate atrophy
- Increase muscle hypertrophy
- Increase muscle strength and endurance
- Resolve activation problems
- Pain relief
- Facilitate bone metabolism
Pillar 4: performance training
Not often used in knee rehab
Individuals can skip pillar 1 and/or 2 if your evaluation suggests that they are able to tolerate the stress of later pillars.
BFR Training as a Bridge Towards High Load Training
BFRT is already being used all over the world to accelerate fatigue and rehab. Not only with elite athletes, but also with the recreational athlete and non-sporter with knee injuries. Doctors and surgeons are already referring to the use of BFR in their patients rehab! Don’t stay behind. It’s not IF, it’s WHEN!
Are you a doctor or a patient and do you want to find a BFR certified physio? LOOK AT www.bfrproviders.com
Find your BFR specialist
BFR COMPLEMENTS BUT DOES NOT REPLACE TRADITIONAL REHAB
Mathias Thoelen
The BFR Pros
If you have any questions, Mathias Thoelen and The BFR Pros are ready for you!

#CHASETHEPUMP!
The BFR Pros are a team of clinicians, coaches and athletes who have combined forces to bring you the real science and tools behind Blood Flow Restriction.
References:
Abe, T., Kearns, C. F., & Sato, Y. (2006). Muscle size and strength are increased following walk training with restricted venous blood flow from the leg muscle, Kaatsu-walk training. Journal of applied physiology, 100(5), 1460-1466.
Abe, T., Fujita, S., Nakajima, T., Sakamaki, M., Ozaki, H., Ogasawara, R., ... & Ishii, N. (2010). Effects of low-intensity cycle training with restricted leg blood flow on thigh muscle volume and VO2max in young men. Journal of sports science & medicine, 9(3), 452.
Bond, C. W., Hackney, K. J., Brown, S. L., & Noonan, B. C. (2019). Blood flow restriction resistance exercise as a rehabilitation modality following orthopaedic surgery: a review of venous thromboembolism risk. journal of orthopaedic & sports physical therapy, 49(1), 17-27.
Centner, C., Jerger, S., Lauber, B., Seynnes, O. R., Friedrich, T., Lolli, D., ... & König, D. (2022). Low-load blood flow restriction and high-load resistance training induce comparable changes in patellar tendon properties.
Constantinou, A., Mamais, I., Papathanasiou, G., Lamnisos, D., & Stasinopoulos, D. (2022). Comparing hip and knee focused exercises versus hip and knee focused exercises with the use of blood flow restriction training in adults with patellofemoral pain. European Journal of physical and rehabilitation Medicine, 58(2), 225.
Cuddeford, T., & Brumitt, J. (2020). In‐season rehabilitation program using blood flow restriction therapy for two decathletes with patellar tendinopathy: A case report. International journal of sports physical therapy, 15(6), 1184.
Formiga, M. F., Fay, R., Hutchinson, S., Locandro, N., Ceballos, A., Lesh, A., ... & Cahalin, L. P. (2020). EFFECT OF AEROBIC EXERCISE TRAINING WITH AND WITHOUT BLOOD FLOW RESTRICTION ON AEROBIC CAPACITY IN HEALTHY YOUNG ADULTS: A SYSTEMATIC REVIEW WITH META-ANALYSIS. International Journal of Sports Physical Therapy, 15(2).
Giles, L., Webster, K. E., McClelland, J., & Cook, J. L. (2017). Quadriceps strengthening with and without blood flow restriction in the treatment of patellofemoral pain: a double-blind randomised trial. British journal of sports medicine, 51(23), 1688-1694.
Hughes, L., Grant, I., & Patterson, S. D. (2021). Aerobic exercise with blood flow restriction causes local and systemic hypoalgesia and increases circulating opioid and endocannabinoid levels. Journal of Applied Physiology, 131(5), 1460-1468.
Hughes, L., Paton, B., Haddad, F., Rosenblatt, B., Gissane, C., & Patterson, S. D. (2018). Comparison of the acute perceptual and blood pressure response to heavy load and light load blood flow restriction resistance exercise in anterior cruciate ligament reconstruction patients and non-injured populations. Physical Therapy in Sport, 33, 54-61.
Hughes, L., & Patterson, S. D. (2020). The effect of blood flow restriction exercise on exercise-induced hypoalgesia and endogenous opioid and endocannabinoid mechanisms of pain modulation. Journal of Applied Physiology, 128(4), 914-924.
Hughes, L., Patterson, S. D., Haddad, F., Rosenblatt, B., Gissane, C., McCarthy, D., ... & Paton, B. (2019a). Examination of the comfort and pain experienced with blood flow restriction training during post-surgery rehabilitation of anterior cruciate ligament reconstruction patients: A UK National Health Service trial. Physical Therapy in Sport, 39, 90-98.
Hughes, L., Rosenblatt, B., Haddad, F., Gissane, C., McCarthy, D., Clarke, T., ... & Patterson, S. D. (2019b). Comparing the effectiveness of blood flow restriction and traditional heavy load resistance training in the post-surgery rehabilitation of anterior cruciate ligament reconstruction patients: a UK National Health Service Randomised Controlled Trial. Sports Medicine, 49(11), 1787-1805.
Hughes, L., Rosenblatt, B., Paton, B., & Patterson, S. D. (2018). Blood flow restriction training in rehabilitation following anterior cruciate ligament reconstructive surgery: A review. Techniques in Orthopaedics, 33(2), 106-113.
Jack, R. A., Lambert, B. S., Hedt, C. A., Delgado, D., Goble, H., & McCulloch, P. C. (2022). Blood Flow Restriction Therapy Preserves Lower Extremity Bone and Muscle Mass After ACL Reconstruction. Sports Health, 19417381221101006.
Korakakis, V., Whiteley, R., & Epameinontidis, K. (2018). Blood flow restriction induces hypoalgesia in recreationally active adult male anterior knee pain patients allowing therapeutic exercise loading. Physical Therapy in Sport, 32, 235-243.
Kotsifaki, R., Korakakis, V., King, E., Barbosa, O., Maree, D., Pantouveris, M., ... & Whiteley, R. (2023). Aspetar clinical practice guideline on rehabilitation after anterior cruciate ligament reconstruction. British Journal of Sports Medicine, 57(9), 500-514
Patterson, S. D., Hughes, L., Warmington, S., Burr, J., Scott, B. R., Owens, J., ... & Loenneke, J. (2019). Blood flow restriction exercise: considerations of methodology, application, and safety. Frontiers in physiology, 10, 533.
Prue, J., Roman, D. P., Giampetruzzi, N. G., Fredericks, A., Lolic, A., Crepeau, A., ... & Weaver, A. P. (2022). Side effects and patient tolerance with the use of blood flow restriction training after ACL reconstruction in adolescents: a pilot study. International Journal of Sports Physical Therapy, 17(3), 347.
Rolnick, N., Kimbrell, K., Cerqueira, M. S., Weatherford, B., & Brandner, C. (2021). Perceived Barriers to Blood Flow Restriction Training. Frontiers in Rehabilitation Sciences, 14.
Skovlund, S. V., Aagaard, P., Larsen, P., Svensson, R. B., Kjaer, M., Magnusson, S. P., & Couppé, C. (2020). The effect of low‐load resistance training with blood flow restriction on chronic patellar tendinopathy—A case series. Translational Sports Medicine, 3(4), 342-352.
Wernbom, M., & Aagaard, P. (2020). Muscle fibre activation and fatigue with low‐load blood flow restricted resistance exercise—An integrative physiology review. Acta Physiologica, 228(1), e13302.
Free access to Jarrod Wade's presentation on Rehabilitation for Match Demands
[spu popup="1088"]
Despite the large amount of knowledge we now have regarding injury prevention of athletes, the shear amount of non-contact injuries that occur each year can be alarming. The balancing act between allowing an athlete to perform at an elite level and keeping them in a rehabilitation program for an extra couple of days can be a decision that keeps the medical team up at night. There are many factors which can contribute to a decision such as this and being pain free is not always a necessity. It has been found that an athlete’s performance will increase with volume and intensity increases, however, with these factors also comes the increased risk of injury. It has been found that an athlete is seventy times more likely to suffer injury if they exceed their individual weekly training threshold. The following article looks to answer some questions in how the medical team may deal with the manipulation and interpretation of an athlete’s load during the during pre, inter and post season.
Pre-season training for elite clubs, is the strength and conditioning programs designed to prepare athletes for an entire competitive season and not just an individual event. For amateur clubs the pre-season may be used for maintenance of fitness in the post season. The development of a well-planned pre-season training program can lead to a decrease in injury risk, increase in mental strength and condition the body for the cues and contacts of a game. The old adage of “train smarter not harder” has changed with the recent evidence produced by Tim Gabbett and Peter Blanch, with the new spin stating: “Train Smarter, Train Hard”.
The premise being that completing short hard training sessions is more beneficial to athletes than those of a longer duration which has the potential to increase injury risk. Training hard with a vehicle like High Speed Running helps to protect physical qualities of an athlete. However, a well-planned pre-season can only be as well planned as the measurement of the athletes load during that pre-season.
Measuring Loads
There are a number of different ways that load can be measured both subjectively and objectively and all with their own pros and cons.
One such way of measuring an athletes training load is through the use of the Acute: Chronic Workload Ratio. The chronic workload is measured over a four week rolling average, while an acute workload can be anything from one training session to one week, depending on the fatigue level of the athlete. The ratio known as the “sweet spot” is between 0.8 and 1.3, this is further supported by the rule of “10% volume increase” which would produce a 1.1. The “Danger Zone” in the Acute: Chronic Ratio is any workload exceeding 1.5, however, there is increased risk for any ratio above a 1.
Another way of measuring athlete load is through Rate of Perceived Exhaustion (RPE) times the duration of the session (minutes). Using this measurement tool allows for not only physical load to be recognized but the mental load being placed on an athlete. If a programmed session is expected to rate a 7 on the RPE scale but the athlete scores the session as 12 then there may be something else worth exploring within the athletes life.
It is suggested that you have 7 days to manage an injury risk for a non-contact presentation. If an athlete is seen to be in the danger zone for too long a period the use of more recovery sessions or complete rest may be required to decrease the physical and mental stressors affecting the athlete. The load variables that have potential to affect the load felt by the athlete are sport specific and can be both intrinsic and extrinsic in nature.
Contributors to Load
There are a large number of factors which can contribute to load accumulation in an athlete and how that load accumulation is attenuated by the tissues of the body. Past injuries are one of the biggest contributors to future injury whether within the same region of tissues or in a separate region as a result of detraining. What was originally an ankle injury which saw an athlete reduce training load for two weeks, can easily lead a vortex of injury in other regions due to deconditioning associated with the reduced game readiness.
Additionally, the bio-mechanics of an athlete cannot be directly correlated to an injury which has not occurred yet – in other words, you cannot predict a specific injury based on bio-mechanical factors that you may visualize. Yes, those bio-mechanical factors can be seen as risk factor for injury but not specifically tied to an individual athlete and the injury they may incur.
Moment in time injuries (ankle sprains/ACLs) and contact injuries of varying degrees will lead to weakness within those tissues and an increase of further injury in the future. This may be a result of “overloaded” tissues relative to their current ability to handle loads – therefore the question is posed again, is it an Overuse Injury, Overload Injury or Training Error which should be the primary umbrella term used to describe these conditions.
The rehabilitation process which has been used to see the athlete return to sport is also important in the contribution to athlete load.
Did the athlete stop all physical activity over the time of injury?
Did the athlete return to training before returning to sport?
Was the athlete returned to their pre-injury chronic load before returning to game play?
Was the athlete 100% ready to return?
If not is the club, player and practitioner willing to take that risk?
There are many more questions that need to be asked and many more which we have not covered here. These decisions are commonly made under pressure to get the player back to field as soon as possible.
Managing Load
So far we have seen what may contribute to an athlete’s load as well as how we can best measure that load in both a subjective and objective format. But how good is that information if we do not have an effective way of managing those risk factors, acute physical load spikes and psychological stressors?
Load should be considered a vehicle, an objective and subjective matter that can drive an athlete towards injury or away from injury. At the end of the day your main destination is “game day performance” or “season performance”, how you reach that destination can be done via a number of routes and selecting the best one is what must be decided upon by the medical staff, athlete and the organization.
When looking to manage load, an athlete’s activity levels should be modified but never ceased. This is to limit detraining, maintain aerobic and anaerobic fitness and continue a base level of their chronic work load. The use of increased aerobic fitness and lower limb strength has been found to reduce an athletes risk of injury. For a long term injury which requires an extensive rehabilitation program it is suggested that workload is increased by 10% per week until the patient reaches their pre-injury chronic workload and are suitable to return to full training.
In conclusion, the monitoring of an athletes load with both subjective and objective measures is essential in the preparation for the competitive season. The development of a well-structured pre-season training plan can bullet proof an athlete not only for a single event but an entire season if completed successfully. A detailed medical history, injury history and lifestyle awareness is important for understanding of how an athlete should prepare for the sporting tasks required of them; from an easy recovery run to a worst case scenario within a single game. It is important to note that an athlete should not stop activity altogether but modify their activities in a way which is most appropriate for their injury.
References
Blanch, P., & Gabbett, T. (2016). Has The Athlete Trained Enough to Return to Play Safely? The Acute: Chronic Workload Ratio Permits Clinicians to Quantify a Players Risk of Subsequent Injury. British Journal of Sports Medicine.
Gabett, T., Hulin, B., Blanch, P., & Whiteley. (2016). High Training Workloads Alone Do Not Cause Sports Injuries: How You Get There Is The Real Issue. British Journal of Sports Medicine.
Halson, S. (2014). Monitoring Training Load To Understand Fatigue In Athletes. SPorts Medicine, 139 - 147.
Saw, A., Main, L., & Gastin, P. (2015). Monitoring The Athlete Training Response: Subjective Self-Reported Measures Trump Commonly Used Objective Measures: A Systematic Review. British Journal Of Sports Medicine, 281 -291.
Firstly, thanks to the SportsMap for asking me to wrote this blog. I hope as least a couple of you out there can take a thing or two from it!
I first enrolled in Physiotherapy with the aim of working in elite sport. Thankfully, due to a combination of having clear goals, working hard and a fair bit of luck, I have managed to work full time in professional sport since 2010. I am often asked by other Physios about how to get a foot in the door in this area. The reality is that with more students enrolling in Physiotherapy courses than ever before, the competition for jobs is only going to get worse. I by no means have all the answers, but these are a few tips that might help you get an opportunity, and then hopefully allow you to make it a success.
I love working in elite sport. However, it can involve long hours, pressure situations, weekend work, dealing with an array of personalities, constant turnover of staff (including perhaps yourself), public criticism, politics and more. In my view all these potentially negatives are far outweighed by the positives, but prior to embarking on this path make sure you understand all that it involves.
HERE ARE MY 16 KEY’s BE SUCCESSFUL WORKING IN ELITE SPORT:
- You need to immerse yourself in the job and be always evolving. In this age of social media there is no excuse for not keeping abreast of the latest in sports science and medicine. From the time you begin university start to attend conferences and courses, & use social media to follow prominent people, journals and other resources that will add to your knowledge.
- Attempt to get experience working in sport as early as possible. I do not agree with the theory that one should work in a hospital first to ‘round out’ their education. Working in a hospital and sport are miles apart. Attempt to get work in a private practice, with good mentors that will take time to educate you and also have links to sporting clubs or organizations.
- Do not be afraid to network. Be prepared to write emails and call people that you think may be able to give you an opportunity. Showing a willingness to learn and work hard is important early in your career.
- The well known book ‘legacy’ states that ‘better people makes better all blacks.’ The same thing could easily be applied to Physio’s. If I am looking to hire someone, it is the impression I get of them as a character that counts for the most.
- Be familiar with the load requirements of the sport, and ensure when rehabilitating a player that you have them prepared to meet these demands.
- Coaches, players and other staff will often ask why you have a certain opinion, or how you came to a particular decision. Be able to justify how you go about things.
- Do not be a know it all. The best Physio’s I have come across are humble, always learning and realize that they do not have all the answers. Be prepared to listen, evolve, seek assistance and do not be offended when someone else challenges your view points.
- Being ‘just’ a physio is not enough. You should have at least a moderate understanding of other areas such as strength and conditioning & nutrition. This will help you be a better Physio and should allow you to build better relationships with staff in these areas… As long as you don’t tell them how to do their job!
- Each player is different. Work closely with other relevant staff such as the doctor and S & C to provide players with an individual physical preparation program that aims to maximize performance and reduce the risk of injury.
- When a player is injured focus on what they CAN do, as opposed to what they can’t. Be creative and always work around the injury. Use the rehab time as an opportunity to not only address the specific injury, but also to work in conjunction with the S & C staff to improve the overall physical characteristics of the athlete.
- Plan well and have key objective markers from early rehab all the way up until clearing a player to return to competition.
- Have a plan, but also be flexible and ready to adapt and deal with challenges and obstacles along the way.
- Ensure the athlete receives the same message from all support staff. Don’t be the guy that undermines the rest of the group and tells the player that you would be approaching things differently or that your colleague is wrong. Debate amongst staff is healthy, but this needs to be done in the correct manner.
- Be organized, document well and prioritize things that you think will best impact performance.
- Enjoy your job. Bring positivity to the group and don’t take yourself too seriously. Maintain high standards and keep professional relationships with players but don’t be afraid to have a laugh when the time is right.
- Maintain a healthy work / life balance. Work hard but also put aside time to relax and pursue interests away from the job. This will help you be more productive when at work and also minimize the risk of burn out.

- Hamish's thoughts on his experiences working as a head Physio in both professional rugby and the AFL
- What to expect from Hamish at the Upper Limb Rehabilitation in Sport course in the Gold Coast
- Posterior dislocation- what are the tell tale signs?
- Where early management is different between posterior & anterior dislocations
- Common imaging findings following both posterior & anterior shoulder dislocations
- Decision making around surgical Vs non surgical management following instability episodes (see further detailed notes below)
- Differences in post surgical management for anterior and posterior repairs
- Post surgical rehabilitation
- Early exercises & targets
- Time based expectations on restoring ROM and strength
- How & when to introduce pushing, pulling and over head
- How and when to take the athlete into venerable positions (Abd/ ER
- Testing or benchmarking in readiness for a return to play
- What is often missed in shoulder rehabilitation
- Contact based conditioning
- Occupation: overhead/manual labour vs sedentary
- Sporting demands – collision sports
- Co-morbidities/physical inactivity – prolongs recovery
- Evidence based surgical indications (reduces the chance of recurrence): Male <25 y/o with traumatic MOI, requires relocation + high functional demands = EBP supports surgical repair. Generally the risk factors from the literature for recurrent instability include: young age (<40 = 13x higher; majority occurring <25), being a male, contact sport. I would also include young females in collision sports in this category. However it is a discussion and as we discussed there is evidence that people in this group can have a positive outcome without surgery.
- Hypermobility:
- I always question the patient about their episode(s) – patients can use the words dislocation and subluxation synonymously. True dislocation or instability in the absence of dislocation. I always I always question the patient around the MOI and do they have imaging evidence of the dislocation (in ED)/needed someone to relocate the shoulder… If their story is accurate for the MOI then I generally believe them when they say their shoulder dislocated. If they haven’t had true dislocation, rather instability episodes – conservative treatment. Especially if you’re dealing with someone who has more mobility than the average (>4 Beighton’s).
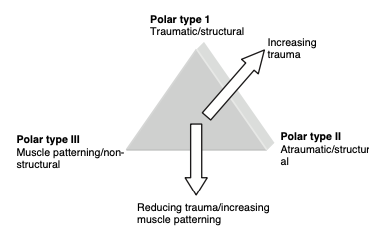
- Traditional classification include the TUBS (Traumatic, unilateral, Bankart, Surgery) and AMBRI (Atraumatic, Multidirectional instability, Bilateral, Recurrent, Inferior Capsular Shift), however this 2nd population doesn’t do as well with surgery as was initially intended with this classification, so conservative path is the best here. A further classification system – The Stanmore Classification (diagram below) further stratifies it into 3 groups and the relationship between trauma, structure and muscle patterning – article attached. In short, group I relates to traumatic dislocation and structural failure, group II with structural laxity that can pre-dispose them to instability with or without trauma, group III to muscle patterning issues causing instability/resting subluxation. Surgery is indicated in group I and only considered in group II with structural failure and who have failed a good rehab program.
 Reference article: Jaggi & Lanbert 2010, Rehabilitation for Shoulder Instability
Reference article: Jaggi & Lanbert 2010, Rehabilitation for Shoulder Instability
- The current state of Sports Physiotherapy
- Tendinopathy
- Spraino & lateral ankle sprain prevention
- Hip ABDuctor & ADDuctor strength and it's relation to groin pain
- Adductor strengthening - why the adductors?
- The Copenhagen- How much is enough and is it sufficient for groin pain prevention?
- How should the groin terminology consensus be used to guide management?
- The HAGOS
- Return to Sport post Hip Arthroscopy
- What are the most important aspects of ACL prevention?
- How to facilitate an optimal learning environment at courses & conference
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
This episode is brought to you by KangaTech & West Coast Health & High Performance (Perth)

- Developments in ACL surgical considerations
- Anatomical risk factors
- Bone bruising in ACL injuries & implications
- Chondral defects of the knee & management strategies
- Surgery Vs non operative management for ACL injuries
- Surgery for degenerative meniscus pathology
- Adolescents & ACL surgery
- Female sports and ACL rupture rates
- Physiotherapy & Rehabilitation considerations with post knee surgery
- PCL surgery
- Posterior lateral corner injuries of the knee
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
This episode is brought to you by KangaTech & West Coast Health & High Performance (Perth)

In this 13th Episode of The Sports MAP Podcast we chat with Chris Perkins about Athletic Lower Back Pain. Chris is s specialist sports Physiotherapist and has worked at the West Coast Eagles (AFL) for past 16 years. He has also worked extensively with world renowned back pain expert Peter O'Sullivan. In this episode we discuss:
- Chris's professional Journey
- The challenges of blending work in professional sport and running a private clinic
- Managing an athletic lower back pain presentation
- Subjective cues
- Objective assessment
- Common contributing factors and how to address these
- Managing work load
- Imaging & red flags
- The use of non threatening language & communication
- Gym based exercises and low back pain
- And more
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
This episode is brought to you by KangaTech & West Coast Health & High Performance (Perth)

In this 12th Episode of The Sports MAP Podcast we chat with Edel Fanning (Phd Candidate) from the Sports Surgery Clinic in Dublin about Shoulder Rehabilitation and RTP from surgery for collision based sports. In this episode we talk to:
- Findings from Edel's recent study in RTP for Shoulder injuries
- Functional testing using force plates to guide decision making
- Isokinetic Vs isometric testing for Rotator cuff strength measures
- Addressing joint position sense in shoulder rehabilitation
- Force plate functional tests Vs ASH test
- Common errors in Shoulder Rehabilitation
- Targeting specific muscle function in Shoulder Rehab
- Laterjet Vs traditional stabilization surgery
- Psychological readiness to return to play
- Edel's key career influences
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
This episode is brought to you by KangaTech & Archies Footwear
Archies are offering all listeners of our podcast a 20% discount on any order. Simply use the code Sports_MAP when ordering from www.archiesfootwear.com

In this 11th Episode of The Sports MAP Network Network we chat with previous Head Physiotherapist for the England Rugby League team Dave O'Sullivan around Syndesmosis Injury Rehabilitation & Dave's Return to Play Systems for lower limb Injury.
- Early focus area's in rehabilitation of a Syndesmosis injury
- Strength assessment & criteria
- Dynamic calf assessment
- Lunge progressions & the importance of the peroneas tertius
- Hopping progressions
- Agility /offline progressions
- Troubleshooting
- Return to running prescription
- Return to play
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
This is episode is brought to you by Archies Footwear
Archies are offering all listeners of our podcast a 20% discount on any order (big or small). Simply use the code Sports_MAP when ordering from www.archiesfootwear.com

In this 8th Episode of the Sports MAP podcast we chat about athlete monitoring and prevention strategies for hamstring and groin injuries in sport with Martin Wollin PhD. In this episode we cover:
- Injury prevention systems- What is primary, secondary & tertiary prevention?
- Adductor strength and ADD:ABD ratio's - relevant to injuries?
- Adductor strength monitoring- key components
- Hamstring power testing as a monitoring tool to mitigate injury risk
- How to manage to an athlete with reduced hamstring strength
- Is hamstring power asymmetry important for injury risk?
- Is monitoring athletes in a team sport setting really worth it?
- Martin's key career influences
- And more
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
This is episode is brought to you by IMeasureU and Vald Performance
Show Notes/ References
- Athlete monitoring: a complementary prevention strategy for groin and hamstring injuries in elite football (PhD Academy Award)
- Effects of match congestion on hamstring strength & lower limb flexibility
- Monitoring the effect of football match congestion on hamstring strength and lower limb flexibility: Potential for secondary injury prevention?
- The effects of football match congestion in an international tournament on hip adductor squeeze strength and pain in elite youth players
- In-season monitoring of hip and groin strength, health and function in elite youth soccer: Implementing an early detection and management strategy over two consecutive seasons
- Reliability of externally fixed dynamometry hamstring strength testing in elite youth football players

/
In this Episode #7 of the Sports MAP Podcast we chat with Enda King around his approach to the Rehabilitation of Complex Athletic Groin Pain using a case example.
- Determining if this athlete is suitable for Rehabilitation
- Assessment protocols
- Addressing & identifying movement based impairments
- Assessment of speed & power in Athletic Groin Pain
- Imaging & the significance of bone marrow edema
- Diagnosis and the entity based approach
- Rehabilitation strength measures
- Return to running & change of direction
- Return to Sport
- Key influences in Enda' career
- And more
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
This is episode is brought to you by IMeasureU and Vald Performance
Show Notes/ References
Clinical & Biomechanical outcomes of Rehabilitation targeting intersegmental control
Enda King Groin Rehabilitation Video Series

/
Shane Kelly is the Head Physiotherapist of the British Athletic Team
In this episode of the Sports Map Podcast, Shane is presented with a case study of an acute calf strain injury and talks us through his process of rehabilitation back to competition levels. Shane touches on the following area's:
- Acute Calf Injury assessment
- Imaging for calf injuries
- Prognostic factors
- Adjuncts for early rehabilitation
- Early loading & building calf capacity
- Foot intrinsic training
- Key criteria in calf rehabilitation
- Return to Run criteria
- Early running prescription
- Training periodization & speed progressions
- Re training acceleration mechanics
- Monitoring response to loads
- Thoughts on ACWR
- Multidisciplinary team involvement for RTS
- Key influences
- And more
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
This is episode is brought to you by IMeasureU
Article
British Athletic Muscle Injury Classification

Scott Epsley is the Director of Physiotherapy & clinical diagnostics at the Philadelphia 76er's in the NBA.
In this episode we chat about:
- Scott's journey from Australia to working in the NBA
- The pro's & cons of working in the NBA
- The Rehabilitation system and structure at the 76er's
- Rehabilitation of 5th metatarsal fractures/ stress fractures
- Using ultrasound to improve diagnostics
- Ultrasound guided dry needling
- Technology advances used in rehabilitation*
- Some interesting early work tendon stiffness in tendinopathy
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via twitter & Facebook.
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
This is episode is brought to you by IMeasureU
