
In this episode of the How I Rehab podcast by Sports MAP we chat with Performance and Rehab manager at New England Patriots, Emidio Pacecca.
Emidio has extensive experience working in elite sporting environments including the Carlton Blues in the AFL, the Australian Institute of Sport (AIS) and Western Force Rugby Union team.
In this episode we cover a range of topics including:
- Emidio’s experience and journey to get to the NFL
- Expectations and responsibilities within an NFL team
- Early strategies around Achilles tendon injuries within the NFL
- Loading protocols
- Isometric loading expectations
- High speed running dosage and hamstring loading
- Strength training expectations across different sports
- Quantifying strength levels
Listen to this Podcast via your favourite platform including Apple, Spotify, Player FM & Stitcher.
You can also VIEW this Podcast on the Sports MAP YouTube channel.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook
As you know, you should begin high-quality rehabilitation immediately after an injury. Everyone with an acute knee injury (e.g. ACL rupture, MCL injury, meniscal tear…) experiences early loss in muscle mass and muscle strength. So the first phase is crucial!
Overuse injuries also require adequate load management to reduce pain and increase load capacity.
Can we reduce these losses and restore them more early with Blood Flow Restriction Training (BFRT)? Can we reduce pain with BFRT?
Yes you heard that right! Blood Flow Restriction Training is able to increase muscle mass and strength with much less weights or NO weights at all. Which is absolutely important to maintain and improve post knee injury to restore daily functioning and participation to sports!
Experts Agree on the Recommendation to Use BFR in ACL Rehab
(Practice guideline Kotsifaki et al., 2023)
Based on the scientific evidence, high intensity strength training is necessary to get these improvements. But all of you know that training with heavy loads is far from possible after an acute knee injury. We need to protect tissue healing and respect the reduced load capacity of the knee! Especially when there are weight bearing restrictions given by the surgeon because of for example a meniscal repair.
So we have no other choice than applying low intensity training in these cases. But almost always muscles aren’t getting into fatigue and thus you aren’t experiencing the feeling of the pump, because of the very high amount of repetitions needed. The pump is actually very important to achieve because we then know that mechanisms are taking place and we are reducing the loss or even gaining muscle mass and strength.
Typically with overuse injuries, patients or athletes experience pain and are unable to tolerate the loading that occurs during training or high intensity strength exercises. Current research is suggesting that BFRT could reduce knee pain (e.g. anterior knee pain, patella femoral pain, patellar tendinopathy). This isn’t the only advantage of BFRT. Imagine your patient or athlete is already able to experience the physiological benefits associated with training at a higher intensity, meaning they are already building muscle mass and strength, or at least maintaining them without performing high intensity strength training.
Researchers found that BFRT can improve cross-sectional area and stiffness of the patellar tendon in healthy individuals. This is interesting to consider regarding the rehab of patellar tendinopathies, but should be further investigated!
BFR is no Magic! It's Pure Exercise Physiology
#CHASETHEPUMP
Besides that, BFR could:
- Reduce loss in bone mineral density and bone mass
- Possibly reduce swelling
- Possibly resolve activation problems
- Maintain or improve aerobic capacity, muscle mass and muscle strength with Aerobic BFRT
- Improve physical functioning and quality of life
- Be used safe in adolescents
LL-BFR Outperforms LL Training without BFR
How should BFRT be applied?
Step 1: is there an indication?
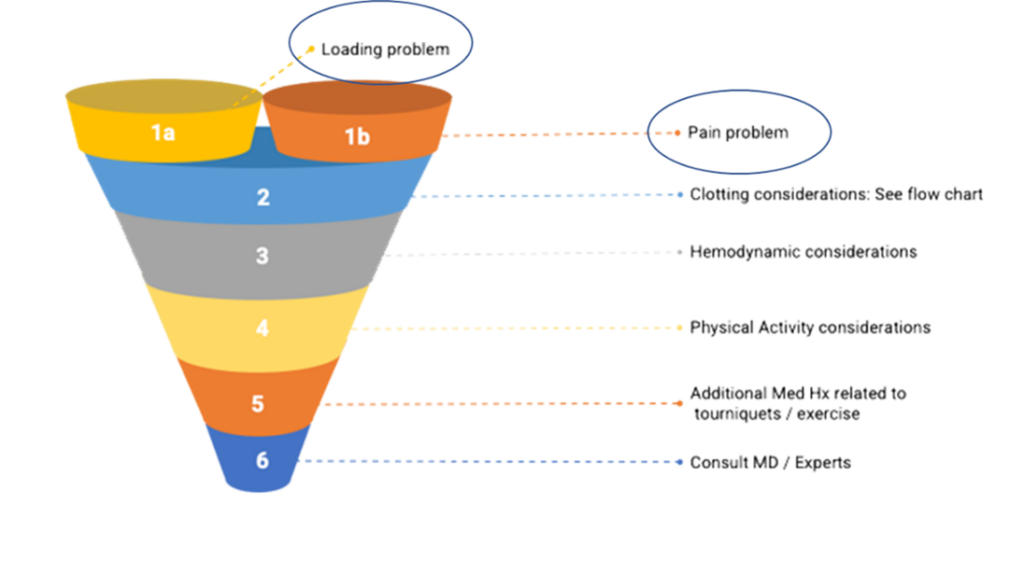
Who is likely an appropriate BFR training candidate? The evidence strongly supports BFR’s use in those patients with either a loading problem or a pain problem.
There is no discussion that there is an indication after for example ACLR or other serious knee injuries. Because load capacity is suppressed and pain is a major factor influencing the knee function.
Step 2: is it safe?
The evidence does not support the assertion that BFR creates blood clots! It seems to reduce the possibility of a blood clot.
BFR is safe if the following requirements are met:
- Medical screening passed
- Rule out absolute contra-indications
- Take into account relative contra-indications
- Blood pressure assessment
- Consult with doctor or expert (when in doubt)
- Applied by an experienced and trained therapist
- Correct protocols and techniques applied
- Use of objective LOP (limb occlusion pressure) assessment and pneumatic cuffs or validated automatic devices
- DON’T USE STRAPS
- DON’T USE PRESSURE BASED ON LEG CIRCUMFERENCE SOLELY
- Choose your cuffs wisely!

Stop Guessing! Start Assessing!
Step 3: write a BFR training program!
Writing a BFR training program includes taking into account medical screening and patient characteristics. Determining the training pressure based on a LOP assessment and prescribing based on the pressure/load continuum are crucial! When necessary, implement strategies to reduce perceptual demands to maintain long-term compliance. Last but not least, think about The Pillars of BFR Training throughout your training and within each session. Use them as a progressive framework/ continuum to applying BFRT from very easy to harder and select the right exercises.
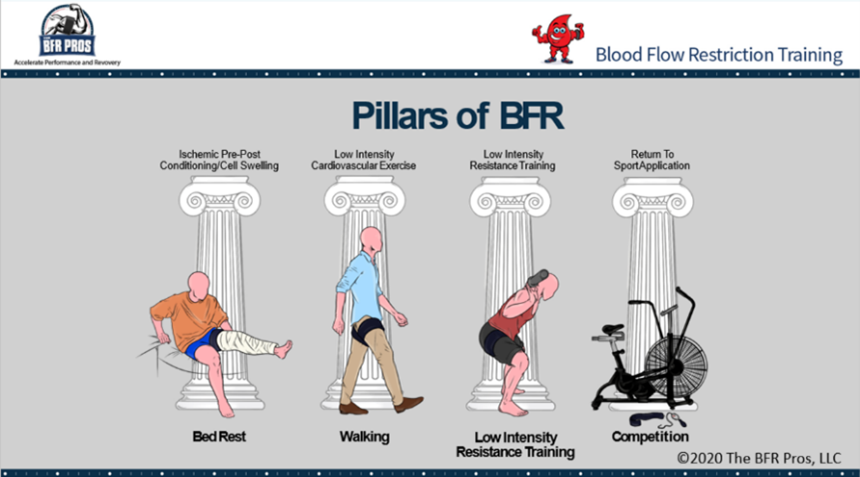
Pillar 1: cell swelling/ passive BFR
Goals of Pillar 1:
- Short familiarization period
- Reduction in atrophy and muscle strength loss
Pillar 2: cardiovascular training
Goals of Pillar 2:
- Increase in muscle mass and strength
- Maintenance or improvement of aerobic capacity
- Pain relief
- Bridge towards pillar 3
Pillar 3: resistance training
Goals of Pillar 3:
- Pursue the same benefits as with traditional high load strength training without all the external mechanical stress
- Attenuate atrophy
- Increase muscle hypertrophy
- Increase muscle strength and endurance
- Resolve activation problems
- Pain relief
- Facilitate bone metabolism
Pillar 4: performance training
Not often used in knee rehab
Individuals can skip pillar 1 and/or 2 if your evaluation suggests that they are able to tolerate the stress of later pillars.
BFR Training as a Bridge Towards High Load Training
BFRT is already being used all over the world to accelerate fatigue and rehab. Not only with elite athletes, but also with the recreational athlete and non-sporter with knee injuries. Doctors and surgeons are already referring to the use of BFR in their patients rehab! Don’t stay behind. It’s not IF, it’s WHEN!
Are you a doctor or a patient and do you want to find a BFR certified physio? LOOK AT www.bfrproviders.com
Find your BFR specialist
BFR COMPLEMENTS BUT DOES NOT REPLACE TRADITIONAL REHAB
Mathias Thoelen
The BFR Pros
If you have any questions, Mathias Thoelen and The BFR Pros are ready for you!

#CHASETHEPUMP!
The BFR Pros are a team of clinicians, coaches and athletes who have combined forces to bring you the real science and tools behind Blood Flow Restriction.
References:
Abe, T., Kearns, C. F., & Sato, Y. (2006). Muscle size and strength are increased following walk training with restricted venous blood flow from the leg muscle, Kaatsu-walk training. Journal of applied physiology, 100(5), 1460-1466.
Abe, T., Fujita, S., Nakajima, T., Sakamaki, M., Ozaki, H., Ogasawara, R., ... & Ishii, N. (2010). Effects of low-intensity cycle training with restricted leg blood flow on thigh muscle volume and VO2max in young men. Journal of sports science & medicine, 9(3), 452.
Bond, C. W., Hackney, K. J., Brown, S. L., & Noonan, B. C. (2019). Blood flow restriction resistance exercise as a rehabilitation modality following orthopaedic surgery: a review of venous thromboembolism risk. journal of orthopaedic & sports physical therapy, 49(1), 17-27.
Centner, C., Jerger, S., Lauber, B., Seynnes, O. R., Friedrich, T., Lolli, D., ... & König, D. (2022). Low-load blood flow restriction and high-load resistance training induce comparable changes in patellar tendon properties.
Constantinou, A., Mamais, I., Papathanasiou, G., Lamnisos, D., & Stasinopoulos, D. (2022). Comparing hip and knee focused exercises versus hip and knee focused exercises with the use of blood flow restriction training in adults with patellofemoral pain. European Journal of physical and rehabilitation Medicine, 58(2), 225.
Cuddeford, T., & Brumitt, J. (2020). In‐season rehabilitation program using blood flow restriction therapy for two decathletes with patellar tendinopathy: A case report. International journal of sports physical therapy, 15(6), 1184.
Formiga, M. F., Fay, R., Hutchinson, S., Locandro, N., Ceballos, A., Lesh, A., ... & Cahalin, L. P. (2020). EFFECT OF AEROBIC EXERCISE TRAINING WITH AND WITHOUT BLOOD FLOW RESTRICTION ON AEROBIC CAPACITY IN HEALTHY YOUNG ADULTS: A SYSTEMATIC REVIEW WITH META-ANALYSIS. International Journal of Sports Physical Therapy, 15(2).
Giles, L., Webster, K. E., McClelland, J., & Cook, J. L. (2017). Quadriceps strengthening with and without blood flow restriction in the treatment of patellofemoral pain: a double-blind randomised trial. British journal of sports medicine, 51(23), 1688-1694.
Hughes, L., Grant, I., & Patterson, S. D. (2021). Aerobic exercise with blood flow restriction causes local and systemic hypoalgesia and increases circulating opioid and endocannabinoid levels. Journal of Applied Physiology, 131(5), 1460-1468.
Hughes, L., Paton, B., Haddad, F., Rosenblatt, B., Gissane, C., & Patterson, S. D. (2018). Comparison of the acute perceptual and blood pressure response to heavy load and light load blood flow restriction resistance exercise in anterior cruciate ligament reconstruction patients and non-injured populations. Physical Therapy in Sport, 33, 54-61.
Hughes, L., & Patterson, S. D. (2020). The effect of blood flow restriction exercise on exercise-induced hypoalgesia and endogenous opioid and endocannabinoid mechanisms of pain modulation. Journal of Applied Physiology, 128(4), 914-924.
Hughes, L., Patterson, S. D., Haddad, F., Rosenblatt, B., Gissane, C., McCarthy, D., ... & Paton, B. (2019a). Examination of the comfort and pain experienced with blood flow restriction training during post-surgery rehabilitation of anterior cruciate ligament reconstruction patients: A UK National Health Service trial. Physical Therapy in Sport, 39, 90-98.
Hughes, L., Rosenblatt, B., Haddad, F., Gissane, C., McCarthy, D., Clarke, T., ... & Patterson, S. D. (2019b). Comparing the effectiveness of blood flow restriction and traditional heavy load resistance training in the post-surgery rehabilitation of anterior cruciate ligament reconstruction patients: a UK National Health Service Randomised Controlled Trial. Sports Medicine, 49(11), 1787-1805.
Hughes, L., Rosenblatt, B., Paton, B., & Patterson, S. D. (2018). Blood flow restriction training in rehabilitation following anterior cruciate ligament reconstructive surgery: A review. Techniques in Orthopaedics, 33(2), 106-113.
Jack, R. A., Lambert, B. S., Hedt, C. A., Delgado, D., Goble, H., & McCulloch, P. C. (2022). Blood Flow Restriction Therapy Preserves Lower Extremity Bone and Muscle Mass After ACL Reconstruction. Sports Health, 19417381221101006.
Korakakis, V., Whiteley, R., & Epameinontidis, K. (2018). Blood flow restriction induces hypoalgesia in recreationally active adult male anterior knee pain patients allowing therapeutic exercise loading. Physical Therapy in Sport, 32, 235-243.
Kotsifaki, R., Korakakis, V., King, E., Barbosa, O., Maree, D., Pantouveris, M., ... & Whiteley, R. (2023). Aspetar clinical practice guideline on rehabilitation after anterior cruciate ligament reconstruction. British Journal of Sports Medicine, 57(9), 500-514
Patterson, S. D., Hughes, L., Warmington, S., Burr, J., Scott, B. R., Owens, J., ... & Loenneke, J. (2019). Blood flow restriction exercise: considerations of methodology, application, and safety. Frontiers in physiology, 10, 533.
Prue, J., Roman, D. P., Giampetruzzi, N. G., Fredericks, A., Lolic, A., Crepeau, A., ... & Weaver, A. P. (2022). Side effects and patient tolerance with the use of blood flow restriction training after ACL reconstruction in adolescents: a pilot study. International Journal of Sports Physical Therapy, 17(3), 347.
Rolnick, N., Kimbrell, K., Cerqueira, M. S., Weatherford, B., & Brandner, C. (2021). Perceived Barriers to Blood Flow Restriction Training. Frontiers in Rehabilitation Sciences, 14.
Skovlund, S. V., Aagaard, P., Larsen, P., Svensson, R. B., Kjaer, M., Magnusson, S. P., & Couppé, C. (2020). The effect of low‐load resistance training with blood flow restriction on chronic patellar tendinopathy—A case series. Translational Sports Medicine, 3(4), 342-352.
Wernbom, M., & Aagaard, P. (2020). Muscle fibre activation and fatigue with low‐load blood flow restricted resistance exercise—An integrative physiology review. Acta Physiologica, 228(1), e13302.
T-Junction injuries of the distal biceps femoris – a more severe variant of hamstring strain injury
Although there are signs of a drop in the number recurrences of hamstring strain injuries (HSIs) in sport[1], it has been long evident both epidemiologically and experientially that these are amongst the most challenging in sport. In fact, since re-injuries have been reported to occur in up to 63% of HSIs[2], it is obvious that it is this recurrence risk underpins the high rates of HSI in sport. If these recurrences could be reduced, it would have an exponential effect on reducing the burden of this injury. What’s more, as these reinjuries typically present having worsened radiologically, they have a significant effect on a club’s injury burden [3].
An important development thus, has been the evolution in imaging classifications that have allowed for bespoke diagnosis, management and rehabilitation. These are particularly important in professional sport where rapid access to MRI common, to meet the pressurized demands of competition and contracts. The widespread adoption of classification systems such as the British Athletics Muscle Injury Classification (BAMIC)[4] mean that modern sports medicine now gives consideration to anatomical location in addition to grading, and can modify expectations accordingly. Although the research so far has been mixed [5, 6], some studies have demonstrated prolonged time to return to play and increased recurrence risk following intramuscular tendon injury in athletes [7-10].
This development has now widely expanded the considerations for clinicians in rehabilitation. Macdonald, McAleer [11] have described a tailored exercise progression with consideration of load, speed and contraction type dependant on BAMIC classification, while Askling, Tengvar [12] has discussed the variation in outcome following stretch and sprint type HSI. Hence, it’s now clear that all HSIs should not be thought to be the same, and they should not be homogenised from a prognostic or management perspective. In order to best mitigate against recurrence, it is necessary to understand the characteristics of each sub-type.
The most frequently injured of the hamstring muscles is the biceps femoris (BF) in running sports [13-15]. While these typically occur at the proximal musculotendinous junction (MTJ), a single retrospective analysis by a Super 15 rugby union team noted higher incidence of distal injuries than had otherwise been previously been reported [14]. Huygaerts, Cos [16] have extensively reviewed the anatomical and morphological features of BF that may predispose it to greater injury risk. As it’s name suggests, BF has two heads – the biarticular long head (LH) forming a conjoint tendon with semitendinosus proximally, and a second monoarticular short head (SH) which functions primarily as a knee flexor. These heads are innervated separately by the common peroneal and tibial nerves respectively.
Importantly, Entwisle, Ling [13] has recently descripted the distal MTJ ‘T-Junction’ of the biceps femoris, formed by a complex confluence of the epimyseal surface of the LH and SH in the distal posterior thigh (Image 1). Injuries to this location have been suggested to be a more severe variant of HSI that should, like intramuscular tendon injuries, be treated as a distinct clinical entity [13, 17].
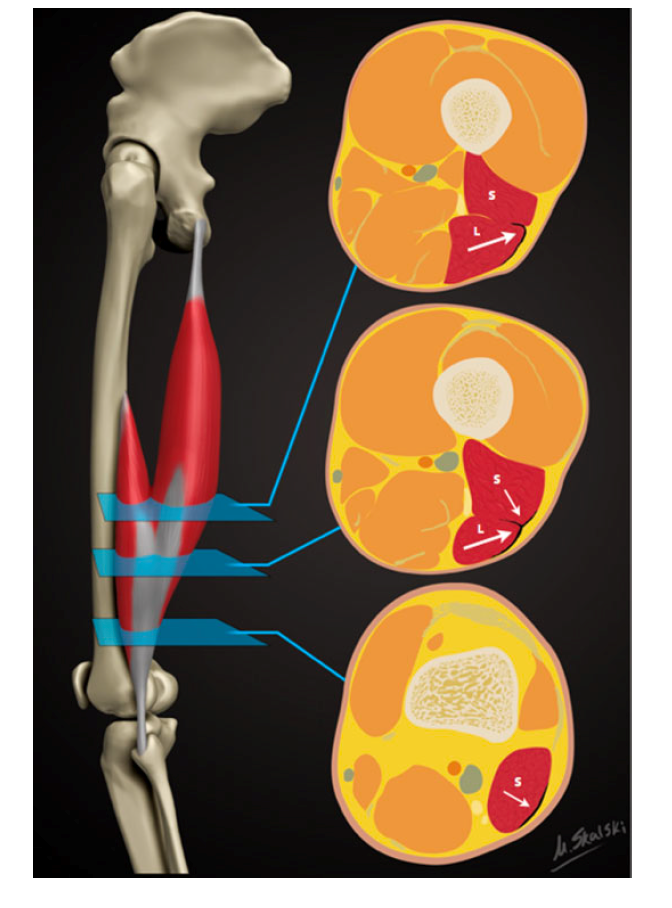
Figure 1: Reproduced from Entwisle, Ling [13]. A schematic demonstrating the sequential axial anatomy of the T junction of the biceps femoris distal musculotendinous junction (MTJ). Proximally, the anterolateral epimyseal surface of the long head (L) condenses to form the proximal portion of the distal MTJ and appears L-, C-, or U-shaped. In the midportion, the opposing epimyseal condensations as the anterolateral aspect of the long head and posterolateral aspect of the short head (S, small arrow) form the DMTJ that appears as a T-shaped structure. Distally, the posterolateral epimyseal condensation of the short head forms the DMTJ and appears as a shallow convex structure.
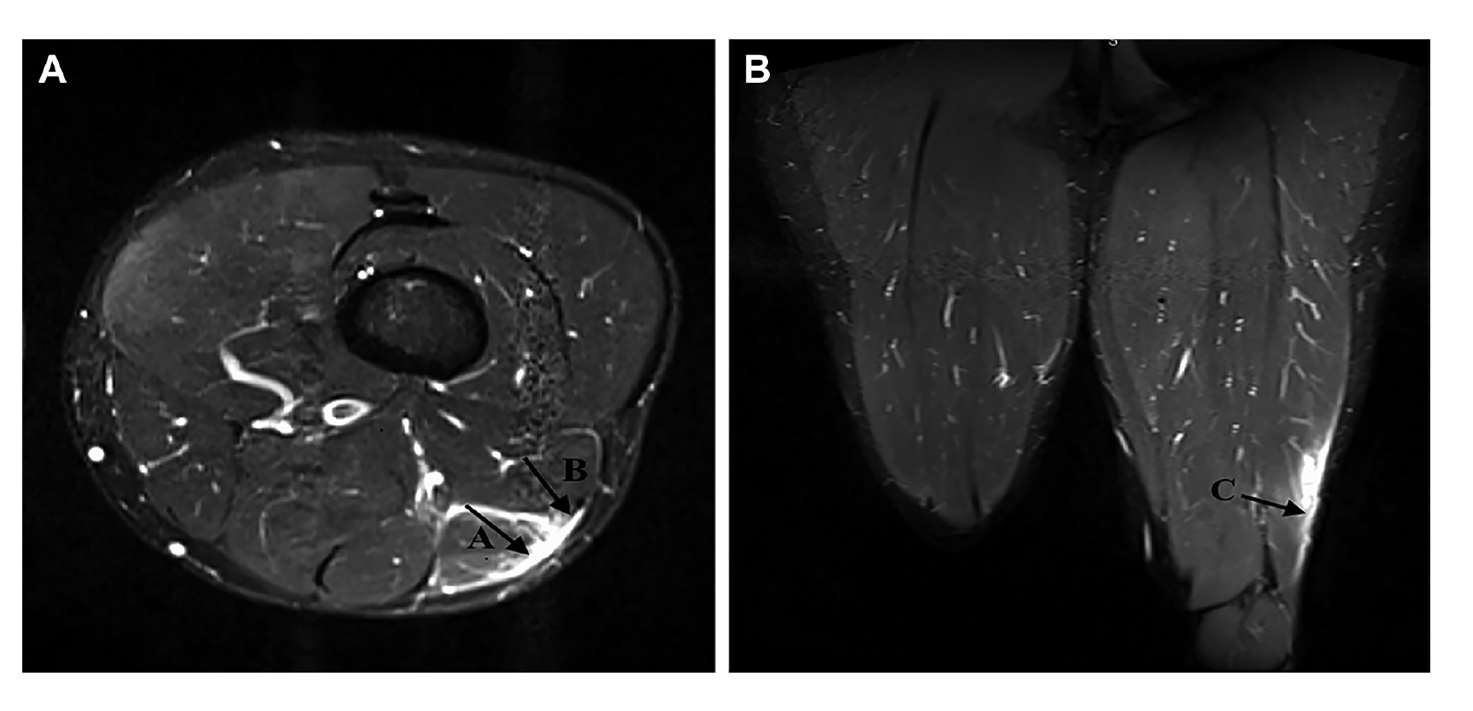
Figure 2: Reproduced from Kayani, Ayuob [17]. Axial section T2-weighted MRI slices showing grade 3 injury to the distal musculotendinous T junction of the biceps femoris with surrounding peritendinous oedema.
Presently, however, there is a vacuum of information to guide us. Firstly, no characteristic mechanism of injury has been described that is associated with T Junction strain. While semimembranosus and proximal free tendon injuries have been shown to occur during overstretch, there is no distinct pattern of T Junction injury. Table 1 outlines the mechanisms of injury of a small subset of athletes who incurred a T Junction injury, but this is by no means an exhaustive analysis of the biomechanical factors involved. Some muscle injury classification systems have been proposed that include the mechanism of injury[18], and these would add value in this case in rising suspicion of such an injury that can only be determined using imaging. With further longitudinal analysis to better understand injury mechanism, preventative strategies – via exercise selection and skill execution – could be designed and trialled.
In addition, no study has described the clinical characteristics of such injuries. There are no proven pathognomic signs that should alert the clinician to the suspected presence of an injury in this location, other than palpation around the distal MTJ. So far, as these injuries can only be identified using MRI and thus, they are most frequently detected in elite sports people. In fact, it is suspected that in many cases these are never identified. This may result in frequent recurrences of BF strains over prolonged periods of time in sub-elite athlete athletes. It has been reported that these injuries become ‘relatively symptom free’ 3-4 weeks following injury, which may lull clinicians into under-estimating the prognosis of such an injury and progressing too rapidly through the return to play process
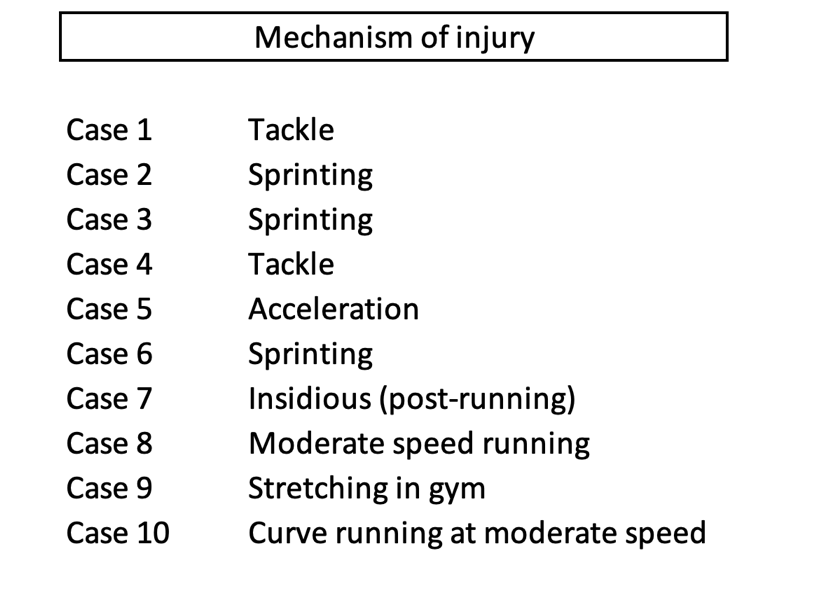
Table 1: Brief description of mechanism of T-Junction injuries observed in 10 cases in a cohort of rugby union players
This early resolution of symptoms may cause the frequency of early recurrences that has been described for this sub-type, with 76% of recurrences occurring within the first 3 months [13]. Incomplete aponeurotic healing remains at 6 weeks following injury [19], so perhaps one principle of management would be a more cautious approach with consideration of the stages of healing.
Periodisation of rehabilitation should give consideration to three keystones – (1) anatomical diagnosis, (2) functional diagnosis or limitations and (3) the demands of ‘return to sport’. Given the nature of the anatomical diagnosis in this case, and the risk of early recurrence, it is proposed that a gentler cadence through the process is best. As with the recommendations for intramuscular tendon injury [11], sprinting activities and exercises involving maximal length, high force and rate of loading should be programmed in a manner that respect immature histological healing at the location of injury.
Consideration should also be given to the distinct characteristics of the distal BF that could be implicated in the poor recovery from injuries in this location as identification of these directs the strength training interventions[20]. The proximal and middle regions of the BFlh have larger pennation angles and greater fascicle lengths than the distal portion [16]. Although this has not prevented the proximal hamstring from being more frequently injured, perhaps the shorter fascicle lengths of the distal hamstring are implicated in poor recovery when injury does occur. Similarly, the distribution of fibre types is not uniform throughout the muscle, with a greater proportion of type 2 muscle fibres existing proximally. This could impact upon the type of training that is deemed optimal for this region.
The duel innervation of the BF is consistently suggested as a potential reason for the high proportion of injuries to this muscle. Given T-junction injuries occur at the confluence of the two heads, it is logical that an asynchrony in co-ordination of the heads could contribute. However, how this can be quantified, and resolved, is unclear and it is only speculative as to what approach could be taken. Macdonald, McAleer [11] suggest isometric exercises as a tool to overcome the neuromuscular inhibition that exists during eccentric exercise following injury[21], and a similar approach may yield benefit in injuries at this confluence.
Recent research has demonstrated the differences in inter-muscular activation during various exercises [20], and has allowed for increasing specificity in rehabilitation. The ‘Nordic hamstring exercise’ and ‘single-leg hip extension’ elicit high activity in the biceps femoris muscle, and thus exercises with these characteristics should be considered important for eliciting an adaptation, while also treated with caution given they are likely to stress this area. Subsequently, Hegyi, Csala [22] has expanded upon this, by demonstrating region specific differences within individual muscles (Figure 3). The eccentric component of the straight knee bridge, upright hip extension conic-pulley and slide leg curl may be most appropriate if attempting to elicit a location specific response in this region, with contraction type adapted dependant on whether the goal is to overcome inhibition (isometric), develop fascicle length or local strength and hypertrophy (eccentric), or simply to induce healing through mechanotherapy. However, again, it is not known whether these injuries occur due to compensation for proximal dysfunction – at which point offloading distally would be the targeted outcome. In the absence of this information, a balanced programme is advised, giving cognisance to inter-muscular and proximal-distal biases, across multiple contraction types.
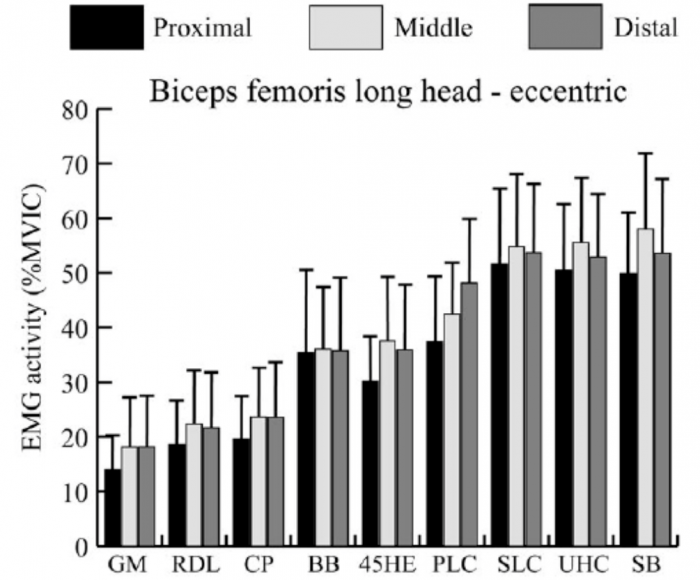
Figure 3: Reproduced from Hegyi, Csala [22]. Mean and standard deviation of the normalized activity level (%MVIC, maximal voluntary isometric contraction) in the proximal, middle, and distal regions of each muscle during the eccentric phase of each exercise. GM, good morning; RDL, unilateral Romanian deadlift; CP, cable pendulum; BB, bent‐knee bridge; 45HE, 45 degree hip extension; PLC, prone leg curl; SLC, slide leg curl; UHC, upright hip extension conic‐pulley; SB, straight‐knee bridge
Given that early recurrence is a key feature is this injury, the pace of progression is critical. If attempting to offload the distal BF, exercises that preferentially activate the medial hamstring or proximal BF may be indicated. In addition, initially restricting range of motion and rate of force development, as well as muscle length across the two involved joints are characteristics of exercise selections that can be manipulated and progressed, while still giving consideration to prioritising the adaptations that might be necessary to prevent recurrence (Table 4).
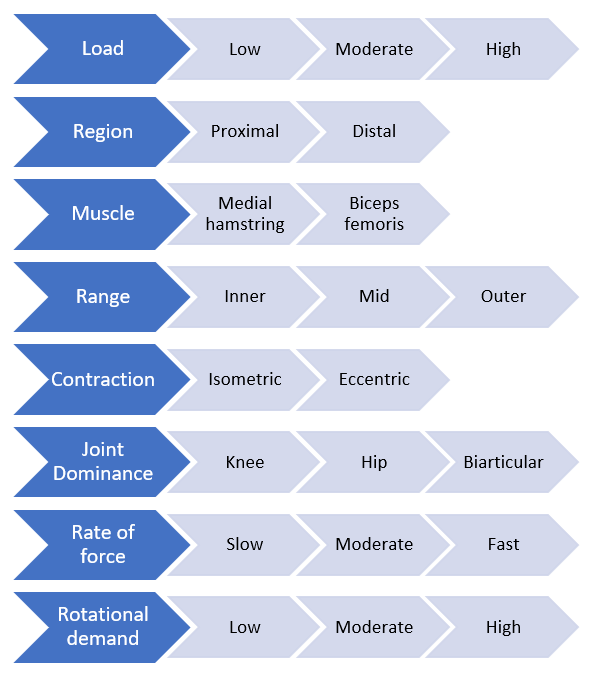
Figure 4: Proposed conceptual progressive loading model specific to a hamstring strain injury
In conclusion, it’s clear that an even more complete approach to rehabilitation is required following T-Junction than for a typical HSI, giving consideration to the structural diagnosis and characteristics of the distal BF. At present however, it remains unclear which anatomical and morphological traits have the greatest influence on injury risk, nor which approaches will generate the most specific and appropriate adaptation. In addition, strategies that help with the identification of these injuries and raise suspicion amongst clinicians would likely improve management of this complex variant of HSI.
References:
- Ekstrand, J., et al., Injury rates decreased in men's professional football: an 18-year prospective cohort study of almost 12 000 injuries sustained during 1.8 million hours of play. Br J Sports Med, 2021.
- de Visser, H.M., et al., Risk factors of recurrent hamstring injuries: a systematic review. Br J Sports Med, 2012. 46(2): p. 124-30.
- Koulouris, G., et al., Magnetic resonance imaging parameters for assessing risk of recurrent hamstring injuries in elite athletes. Am J Sports Med, 2007. 35(9): p. 1500-6.
- Pollock, N., et al., British athletics muscle injury classification: a new grading system. Br J Sports Med, 2014. 48(18): p. 1347-51.
- van der Made, A.D., et al., Intramuscular tendon involvement on MRI has limited value for predicting time to return to play following acute hamstring injury. 2018(1473-0480 (Electronic)).
- van der Made, A.D., et al., Intramuscular tendon injury is not associated with an increased hamstring reinjury rate within 12 months after return to play. 2018(1473-0480 (Electronic)).
- Pollock, N., et al., Time to return to full training is delayed and recurrence rate is higher in intratendinous ('c') acute hamstring injury in elite track and field athletes: clinical application of the British Athletics Muscle Injury Classification. Br J Sports Med, 2016. 50(5): p. 305-10.
- Eggleston, L., M. McMeniman, and C. Engstrom, High-grade intramuscular tendon disruption in acute hamstring injury and return to play in Australian Football players. Scand J Med Sci Sports, 2020.
- Comin, J., et al., Return to competitive play after hamstring injuries involving disruption of the central tendon. Am J Sports Med, 2013. 41(1): p. 111-5.
- Vermeulen, R., et al., Complete resolution of a hamstring intramuscular tendon injury on MRI is not necessary for a clinically successful return to play. Br J Sports Med, 2020.
- Macdonald, B., et al., Hamstring rehabilitation in elite track and field athletes: applying the British Athletics Muscle Injury Classification in clinical practice. Br J Sports Med, 2019. 53(23): p. 1464-1473.
- Askling, C.M., et al., Proximal hamstring strains of stretching type in different sports: injury situations, clinical and magnetic resonance imaging characteristics, and return to sport. Am J Sports Med, 2008. 36(9): p. 1799-804.
- Entwisle, T., et al., Distal Musculotendinous T Junction Injuries of the Biceps Femoris: An MRI Case Review. Orthop J Sports Med, 2017. 5(7): p. 2325967117714998.
- Kenneally-Dabrowski, C., et al., A retrospective analysis of hamstring injuries in elite rugby athletes: More severe injuries are likely to occur at the distal myofascial junction. Phys Ther Sport, 2019. 38: p. 192-198.
- Askling, C.M., et al., Acute first-time hamstring strains during high-speed running: a longitudinal study including clinical and magnetic resonance imaging findings. Am J Sports Med, 2007. 35(2): p. 197-206.
- Huygaerts, S., et al., Does Muscle-Tendon Unit Structure Predispose to Hamstring Strain Injury During Running? A Critical Review. Sports Med, 2021. 51(2): p. 215-224.
- Kayani, B., et al., Surgical Repair of Distal Musculotendinous T Junction Injuries of the Biceps Femoris. Am J Sports Med, 2020. 48(10): p. 2456-2464.
- Valle, X., et al., The MLG-R muscle injury classification for hamstrings. Examples and guidelines for its use. Apunts. Medicina de l'Esport, 2019. 54(202): p. 73-79.
- Jaspers, R.T., et al., Healing of the aponeurosis during recovery from aponeurotomy: Morphological and histological adaptation and related changes in mechanical properties. Journal of Orthopaedic Research, 2005. 23(2): p. 266-273.
- Bourne, M.N., et al., An Evidence-Based Framework for Strengthening Exercises to Prevent Hamstring Injury. Sports Med, 2018. 48(2): p. 251-267.
- Fyfe, J.J., et al., The role of neuromuscular inhibition in hamstring strain injury recurrence. J Electromyogr Kinesiol, 2013. 23(3): p. 523-30.
- Hegyi, A., et al., High-density electromyography activity in various hamstring exercises. Scand J Med Sci Sports, 2019. 29(1): p. 34-43.
- Hegyi, A., et al., Individual Region- and Muscle-specific Hamstring Activity at Different Running Speeds. Med Sci Sports Exerc, 2019. 51(11): p. 2274-2285.
The dream for many sportspeople is to forge a long and successful career as a full-time professional athlete. However, only very few are lucky enough to experience this, and many more athletes across the world end up showcasing their talents as a part-time or semi-professional athlete.
Rather than having the luxury of dedicating most of their time to training and recovery, these athletes are required to work full time jobs (often labour intensive), and then attend training sessions at the end of a 10 hour work day, with training loads very similar to that of an elite athlete.
This obviously poses a massive challenge to the athlete. Having to try and fit in work, training, recovery, family time, social time and sleep all in the space of a 24 hour day.
Managing these athletes can also be a massive challenge for the sports physiotherapists helping them to rehabilitate their injuries and keeping them out on the park.
As we know, load management is an integral part of progressing through a rehabilitation plan, and also helping to reduce the risk of any niggles or injuries. Over the past few years, even with limited resources at semi professional sporting organisations, physios and S+C staff have become much better at monitoring and analysing player loads from a physical, mental and emotional perspective. However, this is where the real challenge lies in dealing with players who work physical jobs throughout the day. For example, take a player who has suffered a calf strain 10 days ago. We can’t expect a player to tell us exactly how many times he has gone up and down the ladder during his work day as an electrician, but should this be a consideration in how much running he does at training that night?
For the athlete playing at this level, at the end of the day, their paid work is a higher priority for the majority of them over their ability to play sport. This often means that rehabilitation from an injury is compromised or lengthened in time, due to the pressures of having to return to work and feed their families. Take the athlete who has had an ACL reconstruction, but also works as a carpenter. The athlete will be eager to return to full time work as soon as they get the all clear from their surgeon, but will being on their feet all day and repetitively squatting cause a knee effusion that will then hinder their ability to perform and progress their strength work?
As their sport might not be their number one priority in their lives as mentioned, training consistency can also be a challenge in dealing with players at this level. Work and family commitments can sometimes clash with training sessions, with missed training sessions affecting their training load for that week, and potentially increasing their risk of injury in the coming weeks.
The emotional toll that having to fit so much into one day can take on the athlete, is also a vital consideration as a sports physiotherapist at this level. We are in a great position as sports physiotherapists to chat to players to ask them how they are coping. Whilst strapping their ankle, we can gain a lot of information about whether or not the athlete has a rough day or period or time, and whether or not they should have a lighter night on the track to help not overload their nervous system.
Many challenges and questions have been posed above, but the number one question is what can we as sport physiotherapists do to help semi-professional athletes overcome these challenges?
In my opinion, the best thing we can do here is to educate our athletes as much as possible, and focus on the ‘big-ticket’ items to allow them to stay at their best for as long as possible.
The ‘big-ticket’ items for me are:
- Sleep – As we know, sleep has been shown to be the most important recovery technique out there for athletes. Sleep is available to both professional and semi-professional athletes, so this has to be a priority.
- Importance of communication – Empower and encourage the athletes to communicate with coaches, S+C staff and physios so we can better monitor how they are dealing with the challenges of being a semi-professional athlete.
- Training consistency – Missing a 10km training session during the week and not making up for it, can often lead to an injury down the track from my experience. It is up to the S+C coach, physio and athlete to formulate a plan as to how to best make up for this session.
I am sure for those sport physiotherapists out there who work at this level with athletes, these are common challenges for you, along with many more that I have not mentioned. Because of these challenges, I find working with these athletes highly enjoyable and rewarding, and I hope you do too!
A big thank you to attendee Luke Nelson for doing a fantastic job in providing this educational summary of our recent course, The Advanced Upper Limb Rehab in Sport.
With a fair share of conferences covering injuries of the lower limb, the SportsMAP Advanced Upper Limb Rehab in Sport event provided a content rich weekend for those wishing to upskill in the management of shoulder, elbow and wrist injuries. Featuring some of the top clinicians in their field, the event did not fail to deliver, with the typical SportsMAP format of combining theory and practical sessions. This blog will present some of the key topics discussed throughout the weekend, and is by no means all the content covered over the 2 days!
Kicking the event off on Day 1 was Andrew McGough, Head Physiotherapist Diving Australia, with “The Sporting Shoulder”.
One of the recurring themes throughout the weekend was the importance of assessing the kinetic chain in athletes with injuries to the upper extremity: for a number of athletic actions (ie. throwing, hitting) the generation of force begins from the ground up. Neglecting to address issues further down the body may be the difference between failure and success in rehabilitating the athlete. Andrew used the case example of a 29 year old Strongman competitor with shoulder pain, who displayed poor trunk control.
“It must be realized that throwing is a whole body activity”
Andrew stressed the importance of both discussing with the athlete and then examining what they CAN and CAN’T do with their presenting complaint. “What can you do? Do that, What can’t you do? Modify that”
Examination of the throwing athlete
Physical examination of the athlete with shoulder pain should be comprehensive to address all potential contributions. This incorporates a full assessment of the kinetic chain. Andrew discussed some of the key tests that should form part of the examination
When assessing flexibility, some tests that should be performed include:
- Shoulder IR/ER range: total range 180 degrees
- Lat dorsi/pec minor length
- Thoracic extension/rotation range
- Cervical ROM
- Combined elevation test: should be able to get above ears
- Knee to wall test
- Hamstring/hip flexor/glut length
- Active straight leg raise
- Hip IR range (especially on lead leg)
Neuromuscular tests
- Rubber duck test: get the athlete to close their eyes, squeeze a squeaky rubber duck and get them to touch it
- Closed kinetic chain test
- Upper limb Y balance test
- Single leg squat (especially ability to load into trail leg)
Strength testing
- Single arm wall push up
- Side plank hold L vs R
- Glut bridge single leg
- Front plank hold
- Int/ext rot in neutral: performed in standing, 3:2 ratio
- Resisted ext and int rotation: can test at different ranges of external/internal rotation
- Testing push and pulls at different positions and ranges
Following assessment, Andrew then discussed the possible intervention and rehab options that are available.
Session 2 saw Kylie Holt, Senior Sports Physio Swimming Australia, present on her area of expertise: the swimmer’s shoulder. Swimmers shoulder is a highly prevalent condition, occurring in 70% of swimmers and with no decrease in incidence in the last 36 years.
Kylie firstly clarified some of the potential contributors to the “swimmer’s shoulder”, with a number of often cited causes shown to be lacking in evidence, or with evidence to the contrary:
- Absolute training volume: no studies linking absolute training volume
- Limitation of ranges specific to swimming (internal rotation >40deg), external rotation (>93, <100): no difference in range with those with pain in Swimming Australia 70 swimmers Holt et al 2017. Not predictive of pain. Those with less humeral torsion were the higher level performers. Relatively ante torted bilaterally, not greatly different from the general population but different from throwing population.
- Scapular dyskinesis: MacLaine 2018. Is important to assess. No necessarily strength related. Is dyskinesia secondary to pain?? Scapular upward rotation/ position is highly variable, don’t bother measuring just YES/NO
- Strength imbalance: Boettcher et al 2019 in press: average ratio 3:2 Int/Ext, those with pain often maintain ratio but decrease strength in both. NOT predictive of pain. Using manual muscle testing to assess tendon health & monitoring.
- Insufficient glenohumeral stability/laxity: vast majority of swimmers have laxity, but not classified as instability. They are just mobile. +ve sulcus sign in 82 of 84 (98%) shoulders examined. We want shoulder movement overhead, stop cueing down and back with shoulders.
Kylie then discussed her yet to be published research of the MRI imaging findings in 60 elite swimmers versus 22 aged matched controls.
Summary of the key findings from this study:
- Tendinopathy is highly prevalent & major findings in swimmers
- Anterior (subscap) and superior (supraspinatus) cuff affected equally: subscapularis (29.2% grade 3) and supraspinatus (30% grade 2) tendinopathic changes, with only 30% showing “normal” tendons in these regions
- Biceps sheath effusion, labral pathology & lesser tubercle oedema not uncommon. 100% of all swimmers have swelling in the long head of biceps, leading to believe that this finding is “normal” in swimmers
- AC joint pathology common
- Subacromial bursa possibly less affected than thought: all subacromial bursa examined were within normal limits
- Early phases of stroke most pain provoking
- Single greatest predictor of tendinopathy in swimmers is years in squad training (especially for subscap tendinopathy).
Findings from this study are not consistent with an external impingement model: In the catch position the subscap is impinging with labrum, and the Supraspinatus is NOT in contact with the acromion. Subacromial external impingement probably less a factor than what previously thought, time for a new model?
"Swimmers Shoulder" Tendinopathy- Anterior superior internal impingement (ASII) and Posterior superior internal impingement (PSII)
- Normal physiological internal contact in high degrees of elevation and internal rotation
- Elite training volume potential to drive pathological response
- Tendinopathy caused by mixed loading ie tensile, compressive & intra-substance shear
- This ASII and PSII explains pathoanatomical findings ie subscapularis, biceps, supraspinatus & intra-articular changes
Things to keep in mind for management of the “Swimmers shoulder”:
- Tendinosis is highly prevalent in swimmers
- Changes in load therefore likely to be an issue (ACWR rather than absolute)
- In many situations not a case of "here now- gone tomorrow"
- Monitor and strengthen the muscle/tendon unit
- Scapular upward rotation likely to be important
- Avoid hyper elevated position where possible (ie. kickboard kicking, chin-ups)
- Are bursal injections as necessary as once thought?
Keeping with the SportMAP mix of theory and practical, it was time to get moving with a breakout into practical workshops.
First up Bruce Rawson, Head Physiotherapist Australian Baseball, took attendees through a throwing rehab workshop. Attendees were fortunate to have former Major League Baseball player, Brad Harman assist in this workshop, giving his unique experience of playing in the majors.
Again reiterating what was taught in the earlier theory, attendees were reminded that throwing is
- Whole body activity
- Complex skill
Therefore, when presented with an injury in the throwing athlete, important to address the 2 above factors.
Fundamentals are important in throwing, and one must not overlook the grip in throwers: if this is not right, then everything else can follow. The correct grip on a ball is 2 fingers on top thumb UNDERNEATH. A common error seen in throwers is the thumb coming up near the index finger, which tends to create a sideways movement when throwing. It is also important to have a gap between the ball and hands
Other key aspects of throwing techniques examined in this workshop were:
- Have the body is squared up side on to target
- Step towards the target not off to the side.
- Ensure that the arm does not winding back before lifting the front leg: they should be simultaneous to help with energy storage.
- Follow through with the thumb down and across the body NOT just across the body
The second workshop with Andrew McGough saw attendees split into small groups and get creative with finding suitable rehabilitative exercises for 2 cases of an injured athlete. What was interesting to observe in this workshop was that pretty much all groups came up with different exercises, which demonstrates the multitude of rehabilitative options we have for the injured athlete.
Day 2
The second day started with Bruce Rawson discussing rehabilitation of the shoulder and elbow in the throwing athlete. In late stage rehab & conditioning it’s important to consider both:
- General conditioning AND
- Throwing specific conditioning
Bruce then discussed some of the key exercises which should be part of a throwers rehabilitation program:
Power (again remember that throwing is from the ground up!):
- Push press
- Hang clean
- Olympic lifts
Throwing creates 1-1.5x bodyweight distraction force through the shoulder, therefore the value of exercises like heavy carries and deadlifts can not be underestimated.
To address trunk rotation some potential exercises that can be used include:
- Medicine ball throw: under arm, over arm focusing more on push
- Tornado ball twist: standing or sitting on floor
- Swinging ball on rope above head
To progress a throwing athlete through throwing progressions, simply increase resistance by increasing distance. Athletes need to “earn the right” To throw hard and often.
Focusing on the injured shoulder is not enough, you must assess the whole chain
Don’t forget the kinetic chain of developing force in the throwing athlete: Each body segment starts accelerating when the previous reaches its peak. Those injured will often have incorrect timing in linking these segments.
Ask the athlete when does their shoulder hurt?
- Before release/cocking phase/acceleration: result = reduced velocity of throw. Check ER ROM
- Release after the throw (velocity ok). Check IR ROM, strength (posterior cuff & capsule)
Bruce then discussed injuries to the elbow in the throwing athlete.
For suspicion of UCL injury at the elbow, it’s important to determine if the ligament is torn or not:tears don’t tend to heal often need surgery.
What protects the UCL? biceps and forearm flexors. Will often see tenderness in distal biceps and forearm as a sign of overload at the elbow.
When assessing the UCL, the standard tests don’t stress the UCL highly enough in throwers, so Bruce uses a “bounce test” in the cocking position. Look for pain reproduction in this position.
Additionally, another test that can be used is getting them in the cocking position and then flexing and extending the elbow, again looking for pain reproduction.
This session then lead into another practical workshop with both Bruce and Andrew demonstrating some of the key exercises that can be used for the throwing athlete.
Next up Phil Cossens, Senior Sports Physio Rowing Australia, explored the unusual wrist & elbow presentations in the athlete.
Posterolateral instability of the elbow
- Can be traumatic and acute or develop over a period of time
- Posterior subluxation of the radial head
- Rotation of ulna/olecranon in fossa
- Severe cases can click
- Mild cases associated with other conditions
Clinical assessment should include:
Table top test
- Palpate and feel for radial head moving posterior
- Positive test is reproduction of their symptoms
Posterolateral rotatory instability test (pivot shift of elbow)
Flex and extend the elbow, feel for movement or reproduction of symptoms.
Osteochondritis dissecans of the capitellum
- Be aware of niggling soreness
- This is a diagnosis that should not be missed
- MRI is essential
- Clicking & locking indicates a worse prognosis
- Weight bearing (ie gymnastics) or throwing
- Palpating capitellar WB surface: flex the elbow (to expose the weight bearing aspect of joint) and you can palpate it
- May have small loss of flexion
- Palpating for swelling in Elbow joint: elbow extended, palpate in olecranon fossa
- Management: conservative management does work, but expect 6-12months
Hyperextension induced posterior impingement
May involve:
- Joint effusion
- Calcification/osteophytes
- Loose bodies
- Ulnar neuritis
- Thickening of triceps tendon
- Thickening of ulnar collateral ligament
(Tyrdal 1999)
Posterior medial impingement or Valgus instability.
- More seen in elbow flexion
TFCC
- Ulnar sided pain with WB and/or traction forces
- Significant injury=instability
- Those with instability will often have a more supinated position of hand on radius and ulna. Distal Ulna may be more prominent
- Pronation of hand may relieve symptoms
Prognosis
There is a continuum from missing 1 week to career ending instability
Overload injuries do well with conservative management if caught early enough
Significant TFC tears require arthroscopic surgery
Extensor carpi ulnaris injury
- Common in racquet sports
Differentials
- Tenosynovitis
- Tendinopathy
- Subluxation: get them to grip then supinate and pronate
- Rupture
Management
- Differs significantly depending on diagnosis (Campbell 2013)
- Consider grip & wrist postures
Intersection syndrome
- More commonly seen in rowers
- Test resisted extension and Finkelstein's test - these tests should be negative before resuming rowing
- More common on inside arm for rowers
Management
- Address technique: excess wrist extension, ulnar deviation & grip
- External factors: rough waters, change grip
- Hard to row through
- Splint, anti inflams, corticosteroids, surgery (Hoy et al 2019)
Attendees then broke into more workshops firstly with Kylie demonstrating assessment of the swimmer, then Craig with rehabilitation of the wrist and elbow.
Some of Kylie’s key tips to assessment of the swimmers shoulder include:
- Scapula assessment: Observe both at rest with arms by side and overhead in streamline position. Not necessarily looking at symmetry of movement, more just that they move
- (Abduction and internal rotation): elbow in armpit, lift elbows up, want to see >140 degrees
- Resisted catch position: look for pain provocation
- Supine internal rotation: 45-60deg
- Supine external rotation: 90+. But greater than 105 is a red flag. You can compensate much easier for a loss of internal rotation vs external rotation
Combined elevation test: hands together, ideal range is humerus 10 degrees above parallel.
This assessment then followed by some good manual therapy techniques to use on the swimmer:
- Prone lat release: arms above head in catch position
Seated lat release: towel around back to grasp lats, then get them to raise arms above head
● Thoracic mobilization
Shifting our attention down to the wrist and elbow, Craig then discussed assessment and rehabilitation of the wrist and elbow.
Some of his go to tests for the elbow include:
Forearm Flexor range test:
● Have 3rd finger facing directly down
● Then slide up the wall as high as you can until the heel of your hand comes off.
● Ensure they don’t rotate the hand to cheat
● Can either measure angle of arm or tape under their fingers
Forearm/shoulder dissociation test:
● Check internal and external rotation holding a dowel with elbow extended: can they disassociate their elbow and shoulder movement.
● They can have their opposite finger on their elbow crease to ensure they are just using more forearm
In regards to rehabilitation for elbow issues, Craig uses pronation & supination exercises a lot: Supinator is an important stabilizer of the elbow.
The anconeus should also not be neglected: Important in supporting the radial lateral component. To palpate this muscle, extend the elbow. Feel the muscle bulk just lateral to the olecranon
UCL thumb injury:
● If they have a high degree of laxity surgery rather than splint
● Usually injured with hyperextension and abduction
● Taping for UCL injuries: Standard Taping is good for abduction but often doesn’t stop extension at thumb. Craig uses a tape underneath in addition to the standard tape.
Extensor tendinopathy
● Craig will often do hands on work on flexor/pronators as tightness in this group can bring the radial head more anterior and potentially increase tendon compression
● Again look for dissociation of forearm & shoulder
● Strengthen supination and pronation as they are important stabilizers.
● Weight bearing exercises are really important as they can often be done pain free and therefore allows the patient to be able to use the arm.
The final sessions of the weekend featured Head Physio from the Melbourne Storm, Meirion Jones, who delved into the management of the “Contact shoulder”.
Some of the key takeaways from these final sessions include:
● Isolated strength: Get volume into cuff with time under tension: 12-15 reps, slow
● Pulling technique: ensure that the shoulder does not dump anteriorly, and allow the scapula to fully retract at the bottom
● Concentric RFD- plyo press, medicine ball throw
● Eccentric RFD- drop and stick
● Reactive RFD- countermovement plyo press
● Proprioceptive rich: isometrics in outer ranges, KB get ups, arm bar trunk rotations, wall walks
Just like we learnt earlier in the weekend with throwing, technique for tackling is also just as important. Early in the rehab, non contact tackling technique drills can be performed, with progression to contact drills when within 15% strength of other side has been achieved.
So as you can see there was a LOT of content covered in the weekend, with this blog the tip of the iceberg. I’d like to thank SportsMAP and the speakers for making this such a great event, and I look forward to attending future events in 2020!
Many thanks to Luke Nelson from Health and High Performance for his contribution with this blog and allowing us to share it our platform.
Free access to Jarrod Wade's presentation on Rehabilitation for Match Demands
[spu popup="1088"]

- Developments in ACL surgical considerations
- Anatomical risk factors
- Bone bruising in ACL injuries & implications
- Chondral defects of the knee & management strategies
- Surgery Vs non operative management for ACL injuries
- Surgery for degenerative meniscus pathology
- Adolescents & ACL surgery
- Female sports and ACL rupture rates
- Physiotherapy & Rehabilitation considerations with post knee surgery
- PCL surgery
- Posterior lateral corner injuries of the knee
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
This episode is brought to you by KangaTech & West Coast Health & High Performance (Perth)

In this 13th Episode of The Sports MAP Podcast we chat with Chris Perkins about Athletic Lower Back Pain. Chris is s specialist sports Physiotherapist and has worked at the West Coast Eagles (AFL) for past 16 years. He has also worked extensively with world renowned back pain expert Peter O'Sullivan. In this episode we discuss:
- Chris's professional Journey
- The challenges of blending work in professional sport and running a private clinic
- Managing an athletic lower back pain presentation
- Subjective cues
- Objective assessment
- Common contributing factors and how to address these
- Managing work load
- Imaging & red flags
- The use of non threatening language & communication
- Gym based exercises and low back pain
- And more
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
This episode is brought to you by KangaTech & West Coast Health & High Performance (Perth)

In this 12th Episode of The Sports MAP Podcast we chat with Edel Fanning (Phd Candidate) from the Sports Surgery Clinic in Dublin about Shoulder Rehabilitation and RTP from surgery for collision based sports. In this episode we talk to:
- Findings from Edel's recent study in RTP for Shoulder injuries
- Functional testing using force plates to guide decision making
- Isokinetic Vs isometric testing for Rotator cuff strength measures
- Addressing joint position sense in shoulder rehabilitation
- Force plate functional tests Vs ASH test
- Common errors in Shoulder Rehabilitation
- Targeting specific muscle function in Shoulder Rehab
- Laterjet Vs traditional stabilization surgery
- Psychological readiness to return to play
- Edel's key career influences
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
This episode is brought to you by KangaTech & Archies Footwear
Archies are offering all listeners of our podcast a 20% discount on any order. Simply use the code Sports_MAP when ordering from www.archiesfootwear.com

In this 11th Episode of The Sports MAP Network Network we chat with previous Head Physiotherapist for the England Rugby League team Dave O'Sullivan around Syndesmosis Injury Rehabilitation & Dave's Return to Play Systems for lower limb Injury.
- Early focus area's in rehabilitation of a Syndesmosis injury
- Strength assessment & criteria
- Dynamic calf assessment
- Lunge progressions & the importance of the peroneas tertius
- Hopping progressions
- Agility /offline progressions
- Troubleshooting
- Return to running prescription
- Return to play
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
This is episode is brought to you by Archies Footwear
Archies are offering all listeners of our podcast a 20% discount on any order (big or small). Simply use the code Sports_MAP when ordering from www.archiesfootwear.com

Welcome to the 10th Episode of the Sports MAP Podcast.
In this Episode we chat to St Kilda Football Club (AFL) Physiotherapist and director of the Hip & Groin Pain Clinic Andrew Wallis on the key aspects in the assessment, diagnosis and management of Hip Dysplasia including:
- What actually is Hip Dysplasia
- How Andrew developed an interest in Hip Dysplasia
- Subjective clues in assessment and key questions to ask patients
- Key objective findings to assist in making a clear diagnosis
- The importance of differentiating FAI and Hip dysplasia
- Pain drivers in hip dysplasia
- Imaging and radiological findings
- Management options available
- Setting expectations
- Conservative management and rehabilitation guidelines
- Return to running and sport
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
This is episode is brought to you by IMeasureU and Vald Performance

In this 9th Episode of the Sports MAP Podcast we chat for a second time with Rehabilitation Specialist from Ireland Enda King about ACL Rehabilitation. Enda touches on many aspects of Rehabilitation with some clinical gold around the following key aspects:
- Key targets/ criteria in early, mid & late stage rehabilitation
- Specific exercise selection
- Errors commonly in rehabilitation and exercise technique
- Isokinetic testing benchmarks
- Linear mechanics and when to commence running
- COD mechanics & how to translate to the field
- Rate of force development prescription and testing
- Key jumping tests
- Changing poor movement patterns in a previously injured athlete
- The influence of fatigue in rehabilitation
- Return to sport
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
This is episode is brought to you by IMeasureU and Vald Performance

/
In this Episode #7 of the Sports MAP Podcast we chat with Enda King around his approach to the Rehabilitation of Complex Athletic Groin Pain using a case example.
- Determining if this athlete is suitable for Rehabilitation
- Assessment protocols
- Addressing & identifying movement based impairments
- Assessment of speed & power in Athletic Groin Pain
- Imaging & the significance of bone marrow edema
- Diagnosis and the entity based approach
- Rehabilitation strength measures
- Return to running & change of direction
- Return to Sport
- Key influences in Enda' career
- And more
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
This is episode is brought to you by IMeasureU and Vald Performance
Show Notes/ References
Clinical & Biomechanical outcomes of Rehabilitation targeting intersegmental control
Enda King Groin Rehabilitation Video Series

/
Shane Kelly is the Head Physiotherapist of the British Athletic Team
In this episode of the Sports Map Podcast, Shane is presented with a case study of an acute calf strain injury and talks us through his process of rehabilitation back to competition levels. Shane touches on the following area's:
- Acute Calf Injury assessment
- Imaging for calf injuries
- Prognostic factors
- Adjuncts for early rehabilitation
- Early loading & building calf capacity
- Foot intrinsic training
- Key criteria in calf rehabilitation
- Return to Run criteria
- Early running prescription
- Training periodization & speed progressions
- Re training acceleration mechanics
- Monitoring response to loads
- Thoughts on ACWR
- Multidisciplinary team involvement for RTS
- Key influences
- And more
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
This is episode is brought to you by IMeasureU
Article
British Athletic Muscle Injury Classification

/
Tim McGrath is the head physiotherapist for St George Illawarra Dragons in the NRL. He holds a PHD in Rehabilitation of the ACL and return to sport and is the clinical director of Elite Physiotherapy in Canberra. In this episode of the Sports MAP Podcast Tim talks to:
- Critical Mechanism of injury factors
- Preventive strategies in team sports
- Common errors in rehabilitation
- Early loading of the quadriceps
- Change of direction mechanics
- Non surgical vs surgical management
- Return to sport testing
- Tim's career influences and world leading ACL practitioners
- And more
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via twitter & Facebook.
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
This is episode is brought to you by IMeasureU

/
Tim Gabbett - Applied Sports Scientist & Load Management Expert talking:
- The pursuit of the unbreakable athlete
- Little wins in rehabilitation
- Return to performance from injury
- Speed requirements for injury prevention & performance
- Working together in High Performance Sports for optimal results
- Strong culture in team sports
- Tim's Leanings from the best sporting organizations in world
- The best athlete Tim has worked with
- Key influences in Tim's career
This episode is brought to you by IMeasureU
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via twitter & Facebook.
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.

/
Jurdan is a world leading expert in the space of hamstring and quadriceps injury prevention and rehabilitation. Jurdan is the current director of Zentrum Sport & consults for some of the best European Soccer Clubs. In this episode Jurdan talks to:
- Key components of this approach to hamstring rehabilitation
- Common errors seen in hamstring rehabilitation
- Power Force Velocity Profiling in hamstring rehabilitation
- Jurdan's greatest professional influences
- What to expect from our Masterclass events with Jurdan in Melbourne and Sydney
This episode is brought to you by IMeasureU
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via twitter & Facebook.
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
