
In this episode of the How I Rehab podcast by Sports MAP we chat with Performance and Rehab manager at New England Patriots, Emidio Pacecca.
Emidio has extensive experience working in elite sporting environments including the Carlton Blues in the AFL, the Australian Institute of Sport (AIS) and Western Force Rugby Union team.
In this episode we cover a range of topics including:
- Emidio’s experience and journey to get to the NFL
- Expectations and responsibilities within an NFL team
- Early strategies around Achilles tendon injuries within the NFL
- Loading protocols
- Isometric loading expectations
- High speed running dosage and hamstring loading
- Strength training expectations across different sports
- Quantifying strength levels
Listen to this Podcast via your favourite platform including Apple, Spotify, Player FM & Stitcher.
You can also VIEW this Podcast on the Sports MAP YouTube channel.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook
As you know, you should begin high-quality rehabilitation immediately after an injury. Everyone with an acute knee injury (e.g. ACL rupture, MCL injury, meniscal tear…) experiences early loss in muscle mass and muscle strength. So the first phase is crucial!
Overuse injuries also require adequate load management to reduce pain and increase load capacity.
Can we reduce these losses and restore them more early with Blood Flow Restriction Training (BFRT)? Can we reduce pain with BFRT?
Yes you heard that right! Blood Flow Restriction Training is able to increase muscle mass and strength with much less weights or NO weights at all. Which is absolutely important to maintain and improve post knee injury to restore daily functioning and participation to sports!
Experts Agree on the Recommendation to Use BFR in ACL Rehab
(Practice guideline Kotsifaki et al., 2023)
Based on the scientific evidence, high intensity strength training is necessary to get these improvements. But all of you know that training with heavy loads is far from possible after an acute knee injury. We need to protect tissue healing and respect the reduced load capacity of the knee! Especially when there are weight bearing restrictions given by the surgeon because of for example a meniscal repair.
So we have no other choice than applying low intensity training in these cases. But almost always muscles aren’t getting into fatigue and thus you aren’t experiencing the feeling of the pump, because of the very high amount of repetitions needed. The pump is actually very important to achieve because we then know that mechanisms are taking place and we are reducing the loss or even gaining muscle mass and strength.
Typically with overuse injuries, patients or athletes experience pain and are unable to tolerate the loading that occurs during training or high intensity strength exercises. Current research is suggesting that BFRT could reduce knee pain (e.g. anterior knee pain, patella femoral pain, patellar tendinopathy). This isn’t the only advantage of BFRT. Imagine your patient or athlete is already able to experience the physiological benefits associated with training at a higher intensity, meaning they are already building muscle mass and strength, or at least maintaining them without performing high intensity strength training.
Researchers found that BFRT can improve cross-sectional area and stiffness of the patellar tendon in healthy individuals. This is interesting to consider regarding the rehab of patellar tendinopathies, but should be further investigated!
BFR is no Magic! It's Pure Exercise Physiology
#CHASETHEPUMP
Besides that, BFR could:
- Reduce loss in bone mineral density and bone mass
- Possibly reduce swelling
- Possibly resolve activation problems
- Maintain or improve aerobic capacity, muscle mass and muscle strength with Aerobic BFRT
- Improve physical functioning and quality of life
- Be used safe in adolescents
LL-BFR Outperforms LL Training without BFR
How should BFRT be applied?
Step 1: is there an indication?
Who is likely an appropriate BFR training candidate? The evidence strongly supports BFR’s use in those patients with either a loading problem or a pain problem.
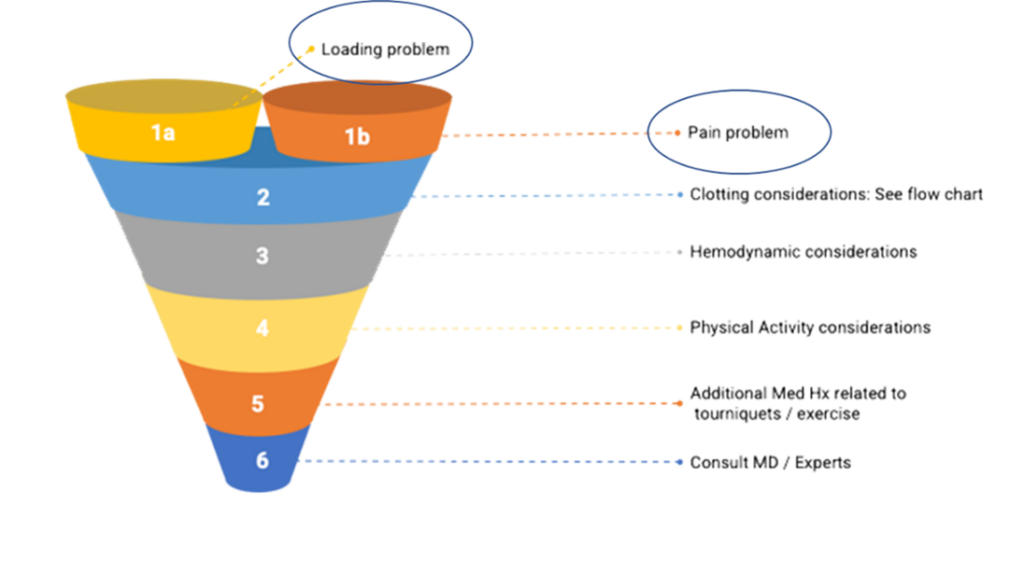
There is no discussion that there is an indication after for example ACLR or other serious knee injuries. Because load capacity is suppressed and pain is a major factor influencing the knee function.
Step 2: is it safe?
The evidence does not support the assertion that BFR creates blood clots! It seems to reduce the possibility of a blood clot.
BFR is safe if the following requirements are met:
- Medical screening passed
- Rule out absolute contra-indications
- Take into account relative contra-indications
- Blood pressure assessment
- Consult with doctor or expert (when in doubt)
- Applied by an experienced and trained therapist
- Correct protocols and techniques applied
- Use of objective LOP (limb occlusion pressure) assessment and pneumatic cuffs or validated automatic devices
- DON’T USE STRAPS
- DON’T USE PRESSURE BASED ON LEG CIRCUMFERENCE SOLELY
- Choose your cuffs wisely!

Stop Guessing! Start Assessing!
Step 3: write a BFR training program!
Writing a BFR training program includes taking into account medical screening and patient characteristics. Determining the training pressure based on a LOP assessment and prescribing based on the pressure/load continuum are crucial! When necessary, implement strategies to reduce perceptual demands to maintain long-term compliance. Last but not least, think about The Pillars of BFR Training throughout your training and within each session. Use them as a progressive framework/ continuum to applying BFRT from very easy to harder and select the right exercises.
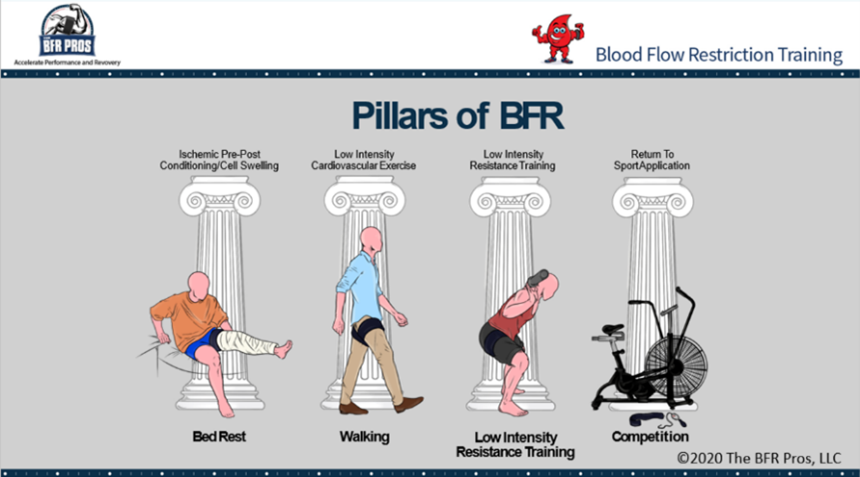
Pillar 1: cell swelling/ passive BFR
Goals of Pillar 1:
- Short familiarization period
- Reduction in atrophy and muscle strength loss
Pillar 2: cardiovascular training
Goals of Pillar 2:
- Increase in muscle mass and strength
- Maintenance or improvement of aerobic capacity
- Pain relief
- Bridge towards pillar 3
Pillar 3: resistance training
Goals of Pillar 3:
- Pursue the same benefits as with traditional high load strength training without all the external mechanical stress
- Attenuate atrophy
- Increase muscle hypertrophy
- Increase muscle strength and endurance
- Resolve activation problems
- Pain relief
- Facilitate bone metabolism
Pillar 4: performance training
Not often used in knee rehab
Individuals can skip pillar 1 and/or 2 if your evaluation suggests that they are able to tolerate the stress of later pillars.
BFR Training as a Bridge Towards High Load Training
BFRT is already being used all over the world to accelerate fatigue and rehab. Not only with elite athletes, but also with the recreational athlete and non-sporter with knee injuries. Doctors and surgeons are already referring to the use of BFR in their patients rehab! Don’t stay behind. It’s not IF, it’s WHEN!
Are you a doctor or a patient and do you want to find a BFR certified physio? LOOK AT www.bfrproviders.com
Find your BFR specialist
BFR COMPLEMENTS BUT DOES NOT REPLACE TRADITIONAL REHAB
Mathias Thoelen
The BFR Pros
If you have any questions, Mathias Thoelen and The BFR Pros are ready for you!

#CHASETHEPUMP!
The BFR Pros are a team of clinicians, coaches and athletes who have combined forces to bring you the real science and tools behind Blood Flow Restriction.
References:
Abe, T., Kearns, C. F., & Sato, Y. (2006). Muscle size and strength are increased following walk training with restricted venous blood flow from the leg muscle, Kaatsu-walk training. Journal of applied physiology, 100(5), 1460-1466.
Abe, T., Fujita, S., Nakajima, T., Sakamaki, M., Ozaki, H., Ogasawara, R., ... & Ishii, N. (2010). Effects of low-intensity cycle training with restricted leg blood flow on thigh muscle volume and VO2max in young men. Journal of sports science & medicine, 9(3), 452.
Bond, C. W., Hackney, K. J., Brown, S. L., & Noonan, B. C. (2019). Blood flow restriction resistance exercise as a rehabilitation modality following orthopaedic surgery: a review of venous thromboembolism risk. journal of orthopaedic & sports physical therapy, 49(1), 17-27.
Centner, C., Jerger, S., Lauber, B., Seynnes, O. R., Friedrich, T., Lolli, D., ... & König, D. (2022). Low-load blood flow restriction and high-load resistance training induce comparable changes in patellar tendon properties.
Constantinou, A., Mamais, I., Papathanasiou, G., Lamnisos, D., & Stasinopoulos, D. (2022). Comparing hip and knee focused exercises versus hip and knee focused exercises with the use of blood flow restriction training in adults with patellofemoral pain. European Journal of physical and rehabilitation Medicine, 58(2), 225.
Cuddeford, T., & Brumitt, J. (2020). In‐season rehabilitation program using blood flow restriction therapy for two decathletes with patellar tendinopathy: A case report. International journal of sports physical therapy, 15(6), 1184.
Formiga, M. F., Fay, R., Hutchinson, S., Locandro, N., Ceballos, A., Lesh, A., ... & Cahalin, L. P. (2020). EFFECT OF AEROBIC EXERCISE TRAINING WITH AND WITHOUT BLOOD FLOW RESTRICTION ON AEROBIC CAPACITY IN HEALTHY YOUNG ADULTS: A SYSTEMATIC REVIEW WITH META-ANALYSIS. International Journal of Sports Physical Therapy, 15(2).
Giles, L., Webster, K. E., McClelland, J., & Cook, J. L. (2017). Quadriceps strengthening with and without blood flow restriction in the treatment of patellofemoral pain: a double-blind randomised trial. British journal of sports medicine, 51(23), 1688-1694.
Hughes, L., Grant, I., & Patterson, S. D. (2021). Aerobic exercise with blood flow restriction causes local and systemic hypoalgesia and increases circulating opioid and endocannabinoid levels. Journal of Applied Physiology, 131(5), 1460-1468.
Hughes, L., Paton, B., Haddad, F., Rosenblatt, B., Gissane, C., & Patterson, S. D. (2018). Comparison of the acute perceptual and blood pressure response to heavy load and light load blood flow restriction resistance exercise in anterior cruciate ligament reconstruction patients and non-injured populations. Physical Therapy in Sport, 33, 54-61.
Hughes, L., & Patterson, S. D. (2020). The effect of blood flow restriction exercise on exercise-induced hypoalgesia and endogenous opioid and endocannabinoid mechanisms of pain modulation. Journal of Applied Physiology, 128(4), 914-924.
Hughes, L., Patterson, S. D., Haddad, F., Rosenblatt, B., Gissane, C., McCarthy, D., ... & Paton, B. (2019a). Examination of the comfort and pain experienced with blood flow restriction training during post-surgery rehabilitation of anterior cruciate ligament reconstruction patients: A UK National Health Service trial. Physical Therapy in Sport, 39, 90-98.
Hughes, L., Rosenblatt, B., Haddad, F., Gissane, C., McCarthy, D., Clarke, T., ... & Patterson, S. D. (2019b). Comparing the effectiveness of blood flow restriction and traditional heavy load resistance training in the post-surgery rehabilitation of anterior cruciate ligament reconstruction patients: a UK National Health Service Randomised Controlled Trial. Sports Medicine, 49(11), 1787-1805.
Hughes, L., Rosenblatt, B., Paton, B., & Patterson, S. D. (2018). Blood flow restriction training in rehabilitation following anterior cruciate ligament reconstructive surgery: A review. Techniques in Orthopaedics, 33(2), 106-113.
Jack, R. A., Lambert, B. S., Hedt, C. A., Delgado, D., Goble, H., & McCulloch, P. C. (2022). Blood Flow Restriction Therapy Preserves Lower Extremity Bone and Muscle Mass After ACL Reconstruction. Sports Health, 19417381221101006.
Korakakis, V., Whiteley, R., & Epameinontidis, K. (2018). Blood flow restriction induces hypoalgesia in recreationally active adult male anterior knee pain patients allowing therapeutic exercise loading. Physical Therapy in Sport, 32, 235-243.
Kotsifaki, R., Korakakis, V., King, E., Barbosa, O., Maree, D., Pantouveris, M., ... & Whiteley, R. (2023). Aspetar clinical practice guideline on rehabilitation after anterior cruciate ligament reconstruction. British Journal of Sports Medicine, 57(9), 500-514
Patterson, S. D., Hughes, L., Warmington, S., Burr, J., Scott, B. R., Owens, J., ... & Loenneke, J. (2019). Blood flow restriction exercise: considerations of methodology, application, and safety. Frontiers in physiology, 10, 533.
Prue, J., Roman, D. P., Giampetruzzi, N. G., Fredericks, A., Lolic, A., Crepeau, A., ... & Weaver, A. P. (2022). Side effects and patient tolerance with the use of blood flow restriction training after ACL reconstruction in adolescents: a pilot study. International Journal of Sports Physical Therapy, 17(3), 347.
Rolnick, N., Kimbrell, K., Cerqueira, M. S., Weatherford, B., & Brandner, C. (2021). Perceived Barriers to Blood Flow Restriction Training. Frontiers in Rehabilitation Sciences, 14.
Skovlund, S. V., Aagaard, P., Larsen, P., Svensson, R. B., Kjaer, M., Magnusson, S. P., & Couppé, C. (2020). The effect of low‐load resistance training with blood flow restriction on chronic patellar tendinopathy—A case series. Translational Sports Medicine, 3(4), 342-352.
Wernbom, M., & Aagaard, P. (2020). Muscle fibre activation and fatigue with low‐load blood flow restricted resistance exercise—An integrative physiology review. Acta Physiologica, 228(1), e13302.
A big thank you to attendee Luke Nelson for doing a fantastic job in providing this educational summary of our recent course, The Advanced Upper Limb Rehab in Sport.
With a fair share of conferences covering injuries of the lower limb, the SportsMAP Advanced Upper Limb Rehab in Sport event provided a content rich weekend for those wishing to upskill in the management of shoulder, elbow and wrist injuries. Featuring some of the top clinicians in their field, the event did not fail to deliver, with the typical SportsMAP format of combining theory and practical sessions. This blog will present some of the key topics discussed throughout the weekend, and is by no means all the content covered over the 2 days!
Kicking the event off on Day 1 was Andrew McGough, Head Physiotherapist Diving Australia, with “The Sporting Shoulder”.
One of the recurring themes throughout the weekend was the importance of assessing the kinetic chain in athletes with injuries to the upper extremity: for a number of athletic actions (ie. throwing, hitting) the generation of force begins from the ground up. Neglecting to address issues further down the body may be the difference between failure and success in rehabilitating the athlete. Andrew used the case example of a 29 year old Strongman competitor with shoulder pain, who displayed poor trunk control.
“It must be realized that throwing is a whole body activity”
Andrew stressed the importance of both discussing with the athlete and then examining what they CAN and CAN’T do with their presenting complaint. “What can you do? Do that, What can’t you do? Modify that”
Examination of the throwing athlete
Physical examination of the athlete with shoulder pain should be comprehensive to address all potential contributions. This incorporates a full assessment of the kinetic chain. Andrew discussed some of the key tests that should form part of the examination
When assessing flexibility, some tests that should be performed include:
- Shoulder IR/ER range: total range 180 degrees
- Lat dorsi/pec minor length
- Thoracic extension/rotation range
- Cervical ROM
- Combined elevation test: should be able to get above ears
- Knee to wall test
- Hamstring/hip flexor/glut length
- Active straight leg raise
- Hip IR range (especially on lead leg)
Neuromuscular tests
- Rubber duck test: get the athlete to close their eyes, squeeze a squeaky rubber duck and get them to touch it
- Closed kinetic chain test
- Upper limb Y balance test
- Single leg squat (especially ability to load into trail leg)
Strength testing
- Single arm wall push up
- Side plank hold L vs R
- Glut bridge single leg
- Front plank hold
- Int/ext rot in neutral: performed in standing, 3:2 ratio
- Resisted ext and int rotation: can test at different ranges of external/internal rotation
- Testing push and pulls at different positions and ranges
Following assessment, Andrew then discussed the possible intervention and rehab options that are available.
Session 2 saw Kylie Holt, Senior Sports Physio Swimming Australia, present on her area of expertise: the swimmer’s shoulder. Swimmers shoulder is a highly prevalent condition, occurring in 70% of swimmers and with no decrease in incidence in the last 36 years.
Kylie firstly clarified some of the potential contributors to the “swimmer’s shoulder”, with a number of often cited causes shown to be lacking in evidence, or with evidence to the contrary:
- Absolute training volume: no studies linking absolute training volume
- Limitation of ranges specific to swimming (internal rotation >40deg), external rotation (>93, <100): no difference in range with those with pain in Swimming Australia 70 swimmers Holt et al 2017. Not predictive of pain. Those with less humeral torsion were the higher level performers. Relatively ante torted bilaterally, not greatly different from the general population but different from throwing population.
- Scapular dyskinesis: MacLaine 2018. Is important to assess. No necessarily strength related. Is dyskinesia secondary to pain?? Scapular upward rotation/ position is highly variable, don’t bother measuring just YES/NO
- Strength imbalance: Boettcher et al 2019 in press: average ratio 3:2 Int/Ext, those with pain often maintain ratio but decrease strength in both. NOT predictive of pain. Using manual muscle testing to assess tendon health & monitoring.
- Insufficient glenohumeral stability/laxity: vast majority of swimmers have laxity, but not classified as instability. They are just mobile. +ve sulcus sign in 82 of 84 (98%) shoulders examined. We want shoulder movement overhead, stop cueing down and back with shoulders.
Kylie then discussed her yet to be published research of the MRI imaging findings in 60 elite swimmers versus 22 aged matched controls.
Summary of the key findings from this study:
- Tendinopathy is highly prevalent & major findings in swimmers
- Anterior (subscap) and superior (supraspinatus) cuff affected equally: subscapularis (29.2% grade 3) and supraspinatus (30% grade 2) tendinopathic changes, with only 30% showing “normal” tendons in these regions
- Biceps sheath effusion, labral pathology & lesser tubercle oedema not uncommon. 100% of all swimmers have swelling in the long head of biceps, leading to believe that this finding is “normal” in swimmers
- AC joint pathology common
- Subacromial bursa possibly less affected than thought: all subacromial bursa examined were within normal limits
- Early phases of stroke most pain provoking
- Single greatest predictor of tendinopathy in swimmers is years in squad training (especially for subscap tendinopathy).
Findings from this study are not consistent with an external impingement model: In the catch position the subscap is impinging with labrum, and the Supraspinatus is NOT in contact with the acromion. Subacromial external impingement probably less a factor than what previously thought, time for a new model?
"Swimmers Shoulder" Tendinopathy- Anterior superior internal impingement (ASII) and Posterior superior internal impingement (PSII)
- Normal physiological internal contact in high degrees of elevation and internal rotation
- Elite training volume potential to drive pathological response
- Tendinopathy caused by mixed loading ie tensile, compressive & intra-substance shear
- This ASII and PSII explains pathoanatomical findings ie subscapularis, biceps, supraspinatus & intra-articular changes
Things to keep in mind for management of the “Swimmers shoulder”:
- Tendinosis is highly prevalent in swimmers
- Changes in load therefore likely to be an issue (ACWR rather than absolute)
- In many situations not a case of "here now- gone tomorrow"
- Monitor and strengthen the muscle/tendon unit
- Scapular upward rotation likely to be important
- Avoid hyper elevated position where possible (ie. kickboard kicking, chin-ups)
- Are bursal injections as necessary as once thought?
Keeping with the SportMAP mix of theory and practical, it was time to get moving with a breakout into practical workshops.
First up Bruce Rawson, Head Physiotherapist Australian Baseball, took attendees through a throwing rehab workshop. Attendees were fortunate to have former Major League Baseball player, Brad Harman assist in this workshop, giving his unique experience of playing in the majors.
Again reiterating what was taught in the earlier theory, attendees were reminded that throwing is
- Whole body activity
- Complex skill
Therefore, when presented with an injury in the throwing athlete, important to address the 2 above factors.
Fundamentals are important in throwing, and one must not overlook the grip in throwers: if this is not right, then everything else can follow. The correct grip on a ball is 2 fingers on top thumb UNDERNEATH. A common error seen in throwers is the thumb coming up near the index finger, which tends to create a sideways movement when throwing. It is also important to have a gap between the ball and hands
Other key aspects of throwing techniques examined in this workshop were:
- Have the body is squared up side on to target
- Step towards the target not off to the side.
- Ensure that the arm does not winding back before lifting the front leg: they should be simultaneous to help with energy storage.
- Follow through with the thumb down and across the body NOT just across the body
The second workshop with Andrew McGough saw attendees split into small groups and get creative with finding suitable rehabilitative exercises for 2 cases of an injured athlete. What was interesting to observe in this workshop was that pretty much all groups came up with different exercises, which demonstrates the multitude of rehabilitative options we have for the injured athlete.
Day 2
The second day started with Bruce Rawson discussing rehabilitation of the shoulder and elbow in the throwing athlete. In late stage rehab & conditioning it’s important to consider both:
- General conditioning AND
- Throwing specific conditioning
Bruce then discussed some of the key exercises which should be part of a throwers rehabilitation program:
Power (again remember that throwing is from the ground up!):
- Push press
- Hang clean
- Olympic lifts
Throwing creates 1-1.5x bodyweight distraction force through the shoulder, therefore the value of exercises like heavy carries and deadlifts can not be underestimated.
To address trunk rotation some potential exercises that can be used include:
- Medicine ball throw: under arm, over arm focusing more on push
- Tornado ball twist: standing or sitting on floor
- Swinging ball on rope above head
To progress a throwing athlete through throwing progressions, simply increase resistance by increasing distance. Athletes need to “earn the right” To throw hard and often.
Focusing on the injured shoulder is not enough, you must assess the whole chain
Don’t forget the kinetic chain of developing force in the throwing athlete: Each body segment starts accelerating when the previous reaches its peak. Those injured will often have incorrect timing in linking these segments.
Ask the athlete when does their shoulder hurt?
- Before release/cocking phase/acceleration: result = reduced velocity of throw. Check ER ROM
- Release after the throw (velocity ok). Check IR ROM, strength (posterior cuff & capsule)
Bruce then discussed injuries to the elbow in the throwing athlete.
For suspicion of UCL injury at the elbow, it’s important to determine if the ligament is torn or not:tears don’t tend to heal often need surgery.
What protects the UCL? biceps and forearm flexors. Will often see tenderness in distal biceps and forearm as a sign of overload at the elbow.
When assessing the UCL, the standard tests don’t stress the UCL highly enough in throwers, so Bruce uses a “bounce test” in the cocking position. Look for pain reproduction in this position.
Additionally, another test that can be used is getting them in the cocking position and then flexing and extending the elbow, again looking for pain reproduction.
This session then lead into another practical workshop with both Bruce and Andrew demonstrating some of the key exercises that can be used for the throwing athlete.
Next up Phil Cossens, Senior Sports Physio Rowing Australia, explored the unusual wrist & elbow presentations in the athlete.
Posterolateral instability of the elbow
- Can be traumatic and acute or develop over a period of time
- Posterior subluxation of the radial head
- Rotation of ulna/olecranon in fossa
- Severe cases can click
- Mild cases associated with other conditions
Clinical assessment should include:
Table top test
- Palpate and feel for radial head moving posterior
- Positive test is reproduction of their symptoms
Posterolateral rotatory instability test (pivot shift of elbow)
Flex and extend the elbow, feel for movement or reproduction of symptoms.
Osteochondritis dissecans of the capitellum
- Be aware of niggling soreness
- This is a diagnosis that should not be missed
- MRI is essential
- Clicking & locking indicates a worse prognosis
- Weight bearing (ie gymnastics) or throwing
- Palpating capitellar WB surface: flex the elbow (to expose the weight bearing aspect of joint) and you can palpate it
- May have small loss of flexion
- Palpating for swelling in Elbow joint: elbow extended, palpate in olecranon fossa
- Management: conservative management does work, but expect 6-12months
Hyperextension induced posterior impingement
May involve:
- Joint effusion
- Calcification/osteophytes
- Loose bodies
- Ulnar neuritis
- Thickening of triceps tendon
- Thickening of ulnar collateral ligament
(Tyrdal 1999)
Posterior medial impingement or Valgus instability.
- More seen in elbow flexion
TFCC
- Ulnar sided pain with WB and/or traction forces
- Significant injury=instability
- Those with instability will often have a more supinated position of hand on radius and ulna. Distal Ulna may be more prominent
- Pronation of hand may relieve symptoms
Prognosis
There is a continuum from missing 1 week to career ending instability
Overload injuries do well with conservative management if caught early enough
Significant TFC tears require arthroscopic surgery
Extensor carpi ulnaris injury
- Common in racquet sports
Differentials
- Tenosynovitis
- Tendinopathy
- Subluxation: get them to grip then supinate and pronate
- Rupture
Management
- Differs significantly depending on diagnosis (Campbell 2013)
- Consider grip & wrist postures
Intersection syndrome
- More commonly seen in rowers
- Test resisted extension and Finkelstein's test - these tests should be negative before resuming rowing
- More common on inside arm for rowers
Management
- Address technique: excess wrist extension, ulnar deviation & grip
- External factors: rough waters, change grip
- Hard to row through
- Splint, anti inflams, corticosteroids, surgery (Hoy et al 2019)
Attendees then broke into more workshops firstly with Kylie demonstrating assessment of the swimmer, then Craig with rehabilitation of the wrist and elbow.
Some of Kylie’s key tips to assessment of the swimmers shoulder include:
- Scapula assessment: Observe both at rest with arms by side and overhead in streamline position. Not necessarily looking at symmetry of movement, more just that they move
- (Abduction and internal rotation): elbow in armpit, lift elbows up, want to see >140 degrees
- Resisted catch position: look for pain provocation
- Supine internal rotation: 45-60deg
- Supine external rotation: 90+. But greater than 105 is a red flag. You can compensate much easier for a loss of internal rotation vs external rotation
Combined elevation test: hands together, ideal range is humerus 10 degrees above parallel.
This assessment then followed by some good manual therapy techniques to use on the swimmer:
- Prone lat release: arms above head in catch position
Seated lat release: towel around back to grasp lats, then get them to raise arms above head
● Thoracic mobilization
Shifting our attention down to the wrist and elbow, Craig then discussed assessment and rehabilitation of the wrist and elbow.
Some of his go to tests for the elbow include:
Forearm Flexor range test:
● Have 3rd finger facing directly down
● Then slide up the wall as high as you can until the heel of your hand comes off.
● Ensure they don’t rotate the hand to cheat
● Can either measure angle of arm or tape under their fingers
Forearm/shoulder dissociation test:
● Check internal and external rotation holding a dowel with elbow extended: can they disassociate their elbow and shoulder movement.
● They can have their opposite finger on their elbow crease to ensure they are just using more forearm
In regards to rehabilitation for elbow issues, Craig uses pronation & supination exercises a lot: Supinator is an important stabilizer of the elbow.
The anconeus should also not be neglected: Important in supporting the radial lateral component. To palpate this muscle, extend the elbow. Feel the muscle bulk just lateral to the olecranon
UCL thumb injury:
● If they have a high degree of laxity surgery rather than splint
● Usually injured with hyperextension and abduction
● Taping for UCL injuries: Standard Taping is good for abduction but often doesn’t stop extension at thumb. Craig uses a tape underneath in addition to the standard tape.
Extensor tendinopathy
● Craig will often do hands on work on flexor/pronators as tightness in this group can bring the radial head more anterior and potentially increase tendon compression
● Again look for dissociation of forearm & shoulder
● Strengthen supination and pronation as they are important stabilizers.
● Weight bearing exercises are really important as they can often be done pain free and therefore allows the patient to be able to use the arm.
The final sessions of the weekend featured Head Physio from the Melbourne Storm, Meirion Jones, who delved into the management of the “Contact shoulder”.
Some of the key takeaways from these final sessions include:
● Isolated strength: Get volume into cuff with time under tension: 12-15 reps, slow
● Pulling technique: ensure that the shoulder does not dump anteriorly, and allow the scapula to fully retract at the bottom
● Concentric RFD- plyo press, medicine ball throw
● Eccentric RFD- drop and stick
● Reactive RFD- countermovement plyo press
● Proprioceptive rich: isometrics in outer ranges, KB get ups, arm bar trunk rotations, wall walks
Just like we learnt earlier in the weekend with throwing, technique for tackling is also just as important. Early in the rehab, non contact tackling technique drills can be performed, with progression to contact drills when within 15% strength of other side has been achieved.
So as you can see there was a LOT of content covered in the weekend, with this blog the tip of the iceberg. I’d like to thank SportsMAP and the speakers for making this such a great event, and I look forward to attending future events in 2020!
Many thanks to Luke Nelson from Health and High Performance for his contribution with this blog and allowing us to share it our platform.
Bruce Hood (Hood 2009) in his book “Supersense: why we believe in the unbelievable” makes a couple of quite pertinent points. He outlines a simple experiment he uses in his presentations where he presents to the audience ‘the pen’ (he admits to stretching the truth here) that Albert Einstein used. The object causes a sense of awe with people wanting to touch it. Immediately after, he offers up an old cardigan which he asks if people would like to try on (maybe that was Albert’s as well). After he has a few takers, he lets it be known that it used to belong to an infamous serial killer -whereupon all of the takers tend to withdraw. As a group, we tend to apply an irrational, supernatural spirituality to objects. This is displayed economically by a painting, supposedly by a grand master being worth millions one day, and nothing the next when described as a fake. Now before all you extremely analytical people jump up and say “I would wear the cardigan” or “I think both paintings are of equal value” this supersense actually extends to the essence of what forms human relationships.
Hood (Hood 2009) further points out that whilst humans do have the capability to make judgements and to reason, there are parts of what make us human and makes our society function that rely on things that go beyond the boundaries of rational analysis. The unconditional love of a mother, the warm feeling you get when you see old friends (in fact having old friends) or being attached to an heirloom from a dead parent, are all examples of emotional based responses that we just accept as ‘normal’. Now again there maybe a few (hopefully only a few) that are still saying, “I feel indifferent about my mother/kids”, “Old friends, what have they done for me lately!” and “I only like new shiny stuff”. If this is the case, it is you that is in the extreme minority. It is argued that it is these traits that have allowed humans to be evolutionarily successful. As individuals in the grand scope of evolutionary time, we are not a particularly hardy example of a species. However as a group that can divide the labour, provide protection and co-operate towards a common goal, we become far more viable. This requires that we form social bonds and these bonds require us to have something more than cold hard reason. We need to believe in something special about the people around us. Our ancestors who were able to create these bonds would have been more successful (finding food, protecting children) and these traits would have entered and then dominated the genetic pool.
In describing the vagaries of evolution theory, in particular evolution of the human cortex, Granger and Lynch in their book “Big brain” point out that we often fall into an evolutionary fallacy (Granger 2008). We often believe we humans are carefully planned, rather than Mother Nature throwing a dice with the DNA and seeing what comes up. Granger and Lynch point out there is no specific reason for why we have 5 fingers (4 or 6 may have been equally as good), but it was a piece of genetic code that was shared about (eventually) amongst a great number of species that worked and didn’t seem to need changing. As a trait becomes more engrained in the success of a species (and then subsequent off-shoots) the less likely there continues to be variations in the code of that trait. Also, it is not only attributes that may bestow some sort of evolutionary advantage, but also those that don’t create too much disadvantage, that can be passed on. Over time these successful (or not too damaging) adaptations form modular patterns within the genetic code that tie together numerous traits and show very little variation. The characteristics of mammals of a spinal cord, head , tail, four limbs, two eyes, two ears and highly similar circulatory, digestive, reproductive and nervous systems, is quite consistent. Furthermore, many of these traits were perfected well before mammals and are borrowed from further back along the evolutionary chain.
Returning to the brain, one of the arguments regarding the evolution of brain size is that increases in brain size are as a result of need, due to changes in behaviour. As our behaviour became more sophisticated, the brain grew to cope with it. Granger and Lynch (Granger 2008) point out that this is somewhat Lamarckian (inheritance of acquired characteristics) and perhaps falling into the above fallacy that our characteristics were carefully planned. They argue that increases in brain size are largely accidental and it is then the behaviour of the species that has to adapt to the rather high biological cost of having a bigger brain. In their words, “Brains are expensive”. Brain cells use up about twice as much energy as the other cells in the body. Bigger brains require longer gestation periods and necessitate longer development to maturity. For humans to survive the genetic code that gave us our big brains had to also encode behaviours that allowed us to pay the cost.
Let’s get back to me on my icebergs and my shivering interpretation of all this. I would argue that for humans to pay the cost of the big brain, the behaviours required would be to create social units that allowed for greater protection and food gathering capabilities. As mentioned earlier, these social units require more than blind brain power to be effective. Whether we call it the “supersense” as described by Hood (Hood 2009) or another name, there appears to be an irrationality and a need to believe, integral in the formation of human emotional bonds. It is within these very traits that the origin of the placebo effect lies. It then may seem attractive to look at the placebo effect as an evolutionary redundancy (did no harm so no need to get rid of it). I think this is a little myopic. We modern humans have been around for about 200,000 years and have been getting sick and injured for most of that time. For a lot of that time, we have had all sorts of healers, shaman and medicine men to help us on our way. However, it is probably only the last seventy years or so (since the advent of evidence-based medicine) that we have any sort of proof that any of the interventions, libations and chants offered up to us has had any effect (helpful or deleterious) (Goldacre 2008).
So, now as I stand somewhat more comfortably than I have for years, with my two icebergs merging into one (those adductors were getting a little stretched). I think we believe because it is far more evolutionary viable to believe than to not believe.
I hope there are no polar bears around here.
References
- Goldacre, B. (2008). Bad science. London, Fourth Estate.
- Granger, G. L. a. R. (2008). Big Brain: The origins and future of human intelligence New York, Palgrave MacMillan.
- Hood, B. M. (2009). Supersense : why we believe in the unbelievable. New York, HarperOne.

- Developments in ACL surgical considerations
- Anatomical risk factors
- Bone bruising in ACL injuries & implications
- Chondral defects of the knee & management strategies
- Surgery Vs non operative management for ACL injuries
- Surgery for degenerative meniscus pathology
- Adolescents & ACL surgery
- Female sports and ACL rupture rates
- Physiotherapy & Rehabilitation considerations with post knee surgery
- PCL surgery
- Posterior lateral corner injuries of the knee
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
This episode is brought to you by KangaTech & West Coast Health & High Performance (Perth)

Welcome to the 10th Episode of the Sports MAP Podcast.
In this Episode we chat to St Kilda Football Club (AFL) Physiotherapist and director of the Hip & Groin Pain Clinic Andrew Wallis on the key aspects in the assessment, diagnosis and management of Hip Dysplasia including:
- What actually is Hip Dysplasia
- How Andrew developed an interest in Hip Dysplasia
- Subjective clues in assessment and key questions to ask patients
- Key objective findings to assist in making a clear diagnosis
- The importance of differentiating FAI and Hip dysplasia
- Pain drivers in hip dysplasia
- Imaging and radiological findings
- Management options available
- Setting expectations
- Conservative management and rehabilitation guidelines
- Return to running and sport
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
This is episode is brought to you by IMeasureU and Vald Performance

In this 9th Episode of the Sports MAP Podcast we chat for a second time with Rehabilitation Specialist from Ireland Enda King about ACL Rehabilitation. Enda touches on many aspects of Rehabilitation with some clinical gold around the following key aspects:
- Key targets/ criteria in early, mid & late stage rehabilitation
- Specific exercise selection
- Errors commonly in rehabilitation and exercise technique
- Isokinetic testing benchmarks
- Linear mechanics and when to commence running
- COD mechanics & how to translate to the field
- Rate of force development prescription and testing
- Key jumping tests
- Changing poor movement patterns in a previously injured athlete
- The influence of fatigue in rehabilitation
- Return to sport
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
This is episode is brought to you by IMeasureU and Vald Performance

In this 8th Episode of the Sports MAP podcast we chat about athlete monitoring and prevention strategies for hamstring and groin injuries in sport with Martin Wollin PhD. In this episode we cover:
- Injury prevention systems- What is primary, secondary & tertiary prevention?
- Adductor strength and ADD:ABD ratio's - relevant to injuries?
- Adductor strength monitoring- key components
- Hamstring power testing as a monitoring tool to mitigate injury risk
- How to manage to an athlete with reduced hamstring strength
- Is hamstring power asymmetry important for injury risk?
- Is monitoring athletes in a team sport setting really worth it?
- Martin's key career influences
- And more
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via Twitter & Facebook.
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
This is episode is brought to you by IMeasureU and Vald Performance
Show Notes/ References
- Athlete monitoring: a complementary prevention strategy for groin and hamstring injuries in elite football (PhD Academy Award)
- Effects of match congestion on hamstring strength & lower limb flexibility
- Monitoring the effect of football match congestion on hamstring strength and lower limb flexibility: Potential for secondary injury prevention?
- The effects of football match congestion in an international tournament on hip adductor squeeze strength and pain in elite youth players
- In-season monitoring of hip and groin strength, health and function in elite youth soccer: Implementing an early detection and management strategy over two consecutive seasons
- Reliability of externally fixed dynamometry hamstring strength testing in elite youth football players

/
Jurdan is a world leading expert in the space of hamstring and quadriceps injury prevention and rehabilitation. Jurdan is the current director of Zentrum Sport & consults for some of the best European Soccer Clubs. In this episode Jurdan talks to:
- Key components of this approach to hamstring rehabilitation
- Common errors seen in hamstring rehabilitation
- Power Force Velocity Profiling in hamstring rehabilitation
- Jurdan's greatest professional influences
- What to expect from our Masterclass events with Jurdan in Melbourne and Sydney
This episode is brought to you by IMeasureU
We hope you enjoy this episode of the Sports MAP Podcast. If you do, please let us know by leaving a review and sharing via twitter & Facebook.
Listen to this Podcast via your favorite platform including Apple, Spotify, Player FM & Stitcher.
