Endurance sport is one of the greatest tests of mental and physical toughness. During a marathon an athlete, on average, will complete 160-200 steps per minute. Whilst running has numerous benefits for our health and wellbeing, it can be monotonous loading on the skeletal system. Bony stress injuries account for up to 20% of running related injuries per year. It is believed that one reason for this is the repetitive overloading on runners’ bones. In comparison, activities involving irregular movements seem to foster greater bone health. The ultimate goal should always be injury prevention, so, should runners incorporate directional movements into their training repertoire for bone health?
Bone is an alive, adaptable, and dynamic structure. Our bone density increases as we grow and by 30 our density is at its peak. After this age we can only maintain what we have. Bone health refers to our bones’ mineral density and quality and is the result of a plethora of factors. In otherwise healthy runners, energy availability, biomechanics, training load and recovery, all play important roles in creating good bone health. Poor bone health can increase the risk of fractures during one’s developmental years and later in life.
There are two main theories that address the way in which our bones are loaded during running. The muscle-bone unit theory refers to the pulling forces created by a muscular contraction. The other references the ground reaction forces through bone when the foot contacts the ground, producing torsional and compressive load. Both mechanisms create macro-trauma which stimulates tissue production and shapes bones geometric structure. However, like other tissues in the body, the activity needs to be progressive otherwise the bone may become accustom and stop adapting. These principles may be used to help runners who may otherwise be stunting adaptation through habitual running load.
In general runners’ bones are healthier than sedentary people. Unfortunately, runners consistently demonstrate lower bone mineral density (BMD) when compared to matched individuals who partake in high impact and irregular movement based sports. A summary of the research of athletes (aged 14-30) found soccer, basketball and volleyball players as well as gymnasts, all displayed greater BMD than those who only ran. A study of young soccer players demonstrated that female players had healthier tibiae than runners and both genders had better density at the spine, femur and calcaneus. In separate studies of track athletes and infantry recruits those who also regularly participated in basketball had up to an 82% reduction in stress fracture risk. Interestingly, in masters athletes those who participated in sprinting had greater BMD than their peers who competed in long distance running. The benefits of diverse loading in youth were also found to protect runners later in life with some up to 50% less likely to sustain a stress fracture.
What seems to be more unclear is the ideal dosage for bony loading. Bone regeneration cycles are suggested to take 3-8months. Studies of humans, mice and turkeys found significant changes after as little as 3 weeks of a jump program. Repetition amount also widely varied between studies from 30 - 350 cycles per week. A study of adolescent females found that a 9-month plyometric program improved only greater trochanter bone strength. Another found plyometric training only benefited those who participated in low osteogenic sports such as swimming. Studies on structure found that rate, magnitude and activity resulted in site specific changes, however, no optimal values for load were presented. No well-known study was found to investigate an irregular, directional and high impact, loading program for the reduction of fracture risk in endurance runners.
It is important to note there are many other factors which influence bone health that have not been explored here. The body needs a plentiful supply of vitamin D and Calcium to build strong bone. To create an optimal environment for this rest and good sleep are also essential. For distance runners who are constantly in a state of low energy availability, bone loading has been found to have little strengthening effects and can be somewhat detrimental if added in addition to their normal training.
Runners want to run. Convincing them to do otherwise continues to remain a great challenge for clinicians, however, it would seem that some variety may strengthen their bones. Youth runners should be encouraged to participate in a variety of sports. Once specialisation occurs, a runner may benefit from incorporating direction and plyometric loading into their training. Unfortunately, the optimal dosage for this is largely unknown.
References
Beck, B. R., Daly, R. M., Singh, M. A. F., & Taaffe, D. R. (2017). Exercise and Sports Science Australia (ESSA) position statement on exercise prescription for the prevention and management of osteoporosis. Journal of Science and Medicine in Sport, 20(5), 438-445.
Gómez Bruton, A., Matute-Llorente, Á., González-Agüero, A., Casajus, J., & Vicente-Rodríguez, G. (2017). Plyometric exercise and bone health in children and adolescents: a systematic review.
Gómez-Cabello, A., Ara, I., González-Agüero, A., Casajús, J. A., & Vicente-Rodríguez, G. (2012). Effects of training on bone mass in older adults: a systematic review. Sports Med, 42(4), 301-325.
Hart, N. H., Nimphius, S., Rantalainen, T., Ireland, A., Siafarikas, A., & Newton, R. U. (2017). Mechanical basis of bone strength: influence of bone material, bone structure and muscle action. Journal of musculoskeletal & neuronal interactions, 17(3), 114-139.
Hong, A. R., & Kim, S. W. (2018). Effects of Resistance Exercise on Bone Health. Endocrinology and metabolism (Seoul, Korea), 33(4), 435-444. doi:10.3803/EnM.2018.33.4.435
Kato, T., Terashima, T., Yamashita, T., Hatanaka, Y., Honda, A., & Umemura, Y. (2006). Effect of low-repetition jump training on bone mineral density in young women. Journal of Applied Physiology, 100(3), 839-843.
Nattiv, A. (2000). Stress fractures and bone health in track and field athletes. J Sci Med Sport, 3(3), 268-279.
Scofield, K. L., & Hecht, S. (2012). Bone health in endurance athletes: runners, cyclists, and swimmers. Curr Sports Med Rep, 11(6), 328-334.
Tenforde, A. S., & Fredericson, M. (2011). Influence of sports participation on bone health in the young athlete: a review of the literature. Pm r, 3(9), 861-867.
Tenforde, A. S., Sainani, K. L., Carter Sayres, L., Milgrom, C., & Fredericson, M. (2015). Participation in ball sports may represent a prehabilitation strategy to prevent future stress fractures and promote bone health in young athletes. Pm r, 7(2), 222-225.
Vlachopoulos, D., Barker, A. R., Ubago-Guisado, E., Williams, C. A., & Gracia-Marco, L. (2018). The effect of a high-impact jumping intervention on bone mass, bone stiffness and fitness parameters in adolescent athletes. Archives of osteoporosis, 13(1), 128-128.
Witzke, K., & Snow, C. (2000). Effects of plyometric jump training on bone mass in adolescent girls. Medicine and science in sports and exercise, 32, 1051-1057.
Wright, A. A., Taylor, J. B., Ford, K. R., Siska, L., & Smoliga, J. M. (2015). Risk factors associated with lower extremity stress fractures in runners: a systematic review with meta-analysis. British Journal of Sports Medicine, 49(23), 1517.
T-Junction injuries of the distal biceps femoris – a more severe variant of hamstring strain injury
Although there are signs of a drop in the number recurrences of hamstring strain injuries (HSIs) in sport[1], it has been long evident both epidemiologically and experientially that these are amongst the most challenging in sport. In fact, since re-injuries have been reported to occur in up to 63% of HSIs[2], it is obvious that it is this recurrence risk underpins the high rates of HSI in sport. If these recurrences could be reduced, it would have an exponential effect on reducing the burden of this injury. What’s more, as these reinjuries typically present having worsened radiologically, they have a significant effect on a club’s injury burden [3].
An important development thus, has been the evolution in imaging classifications that have allowed for bespoke diagnosis, management and rehabilitation. These are particularly important in professional sport where rapid access to MRI common, to meet the pressurized demands of competition and contracts. The widespread adoption of classification systems such as the British Athletics Muscle Injury Classification (BAMIC)[4] mean that modern sports medicine now gives consideration to anatomical location in addition to grading, and can modify expectations accordingly. Although the research so far has been mixed [5, 6], some studies have demonstrated prolonged time to return to play and increased recurrence risk following intramuscular tendon injury in athletes [7-10].
This development has now widely expanded the considerations for clinicians in rehabilitation. Macdonald, McAleer [11] have described a tailored exercise progression with consideration of load, speed and contraction type dependant on BAMIC classification, while Askling, Tengvar [12] has discussed the variation in outcome following stretch and sprint type HSI. Hence, it’s now clear that all HSIs should not be thought to be the same, and they should not be homogenised from a prognostic or management perspective. In order to best mitigate against recurrence, it is necessary to understand the characteristics of each sub-type.
The most frequently injured of the hamstring muscles is the biceps femoris (BF) in running sports [13-15]. While these typically occur at the proximal musculotendinous junction (MTJ), a single retrospective analysis by a Super 15 rugby union team noted higher incidence of distal injuries than had otherwise been previously been reported [14]. Huygaerts, Cos [16] have extensively reviewed the anatomical and morphological features of BF that may predispose it to greater injury risk. As it’s name suggests, BF has two heads – the biarticular long head (LH) forming a conjoint tendon with semitendinosus proximally, and a second monoarticular short head (SH) which functions primarily as a knee flexor. These heads are innervated separately by the common peroneal and tibial nerves respectively.
Importantly, Entwisle, Ling [13] has recently descripted the distal MTJ ‘T-Junction’ of the biceps femoris, formed by a complex confluence of the epimyseal surface of the LH and SH in the distal posterior thigh (Image 1). Injuries to this location have been suggested to be a more severe variant of HSI that should, like intramuscular tendon injuries, be treated as a distinct clinical entity [13, 17].
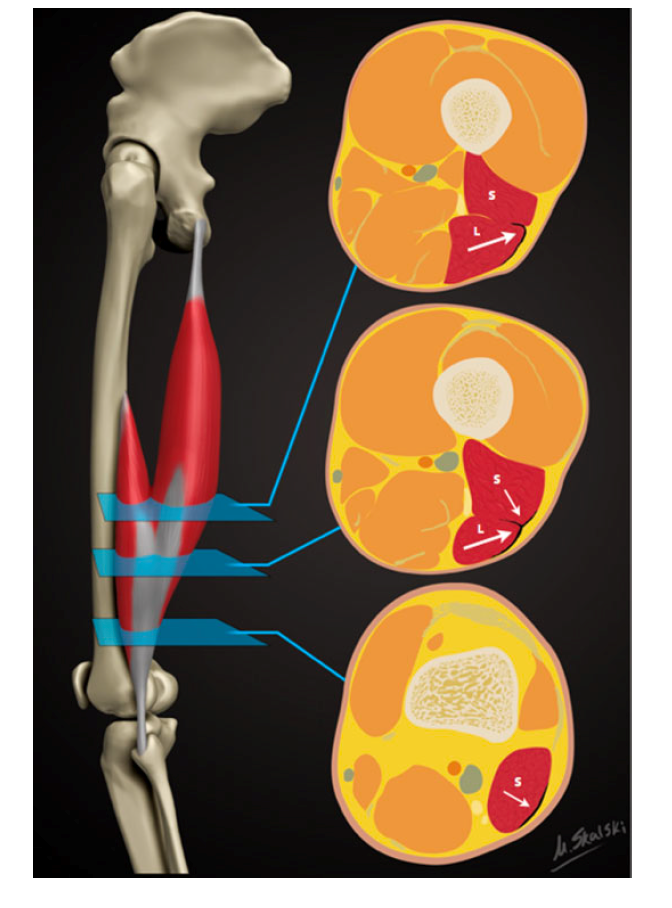
Figure 1: Reproduced from Entwisle, Ling [13]. A schematic demonstrating the sequential axial anatomy of the T junction of the biceps femoris distal musculotendinous junction (MTJ). Proximally, the anterolateral epimyseal surface of the long head (L) condenses to form the proximal portion of the distal MTJ and appears L-, C-, or U-shaped. In the midportion, the opposing epimyseal condensations as the anterolateral aspect of the long head and posterolateral aspect of the short head (S, small arrow) form the DMTJ that appears as a T-shaped structure. Distally, the posterolateral epimyseal condensation of the short head forms the DMTJ and appears as a shallow convex structure.
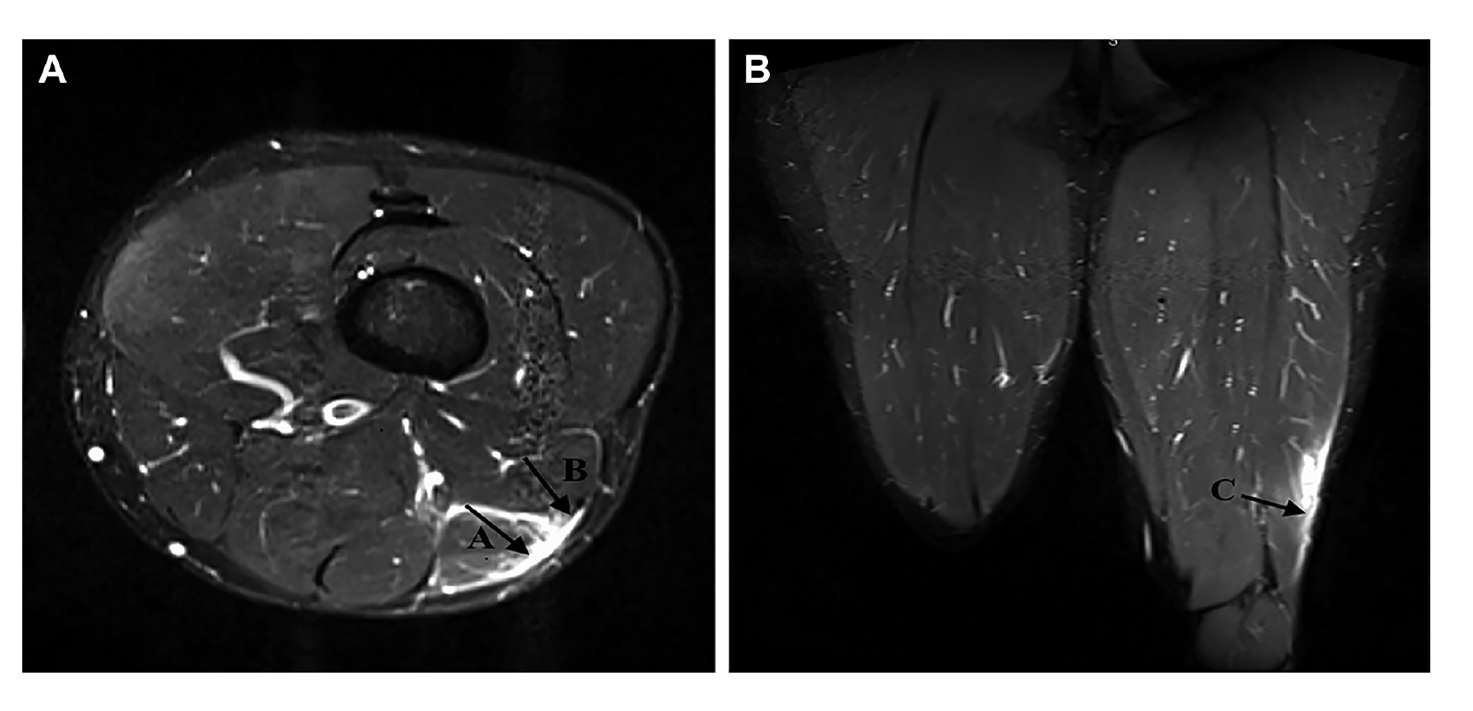
Figure 2: Reproduced from Kayani, Ayuob [17]. Axial section T2-weighted MRI slices showing grade 3 injury to the distal musculotendinous T junction of the biceps femoris with surrounding peritendinous oedema.
Presently, however, there is a vacuum of information to guide us. Firstly, no characteristic mechanism of injury has been described that is associated with T Junction strain. While semimembranosus and proximal free tendon injuries have been shown to occur during overstretch, there is no distinct pattern of T Junction injury. Table 1 outlines the mechanisms of injury of a small subset of athletes who incurred a T Junction injury, but this is by no means an exhaustive analysis of the biomechanical factors involved. Some muscle injury classification systems have been proposed that include the mechanism of injury[18], and these would add value in this case in rising suspicion of such an injury that can only be determined using imaging. With further longitudinal analysis to better understand injury mechanism, preventative strategies – via exercise selection and skill execution – could be designed and trialled.
In addition, no study has described the clinical characteristics of such injuries. There are no proven pathognomic signs that should alert the clinician to the suspected presence of an injury in this location, other than palpation around the distal MTJ. So far, as these injuries can only be identified using MRI and thus, they are most frequently detected in elite sports people. In fact, it is suspected that in many cases these are never identified. This may result in frequent recurrences of BF strains over prolonged periods of time in sub-elite athlete athletes. It has been reported that these injuries become ‘relatively symptom free’ 3-4 weeks following injury, which may lull clinicians into under-estimating the prognosis of such an injury and progressing too rapidly through the return to play process
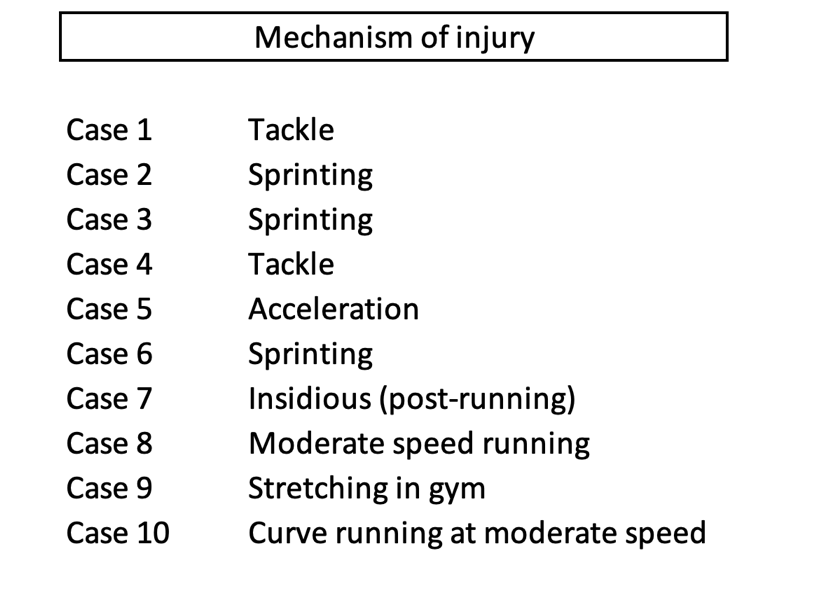
Table 1: Brief description of mechanism of T-Junction injuries observed in 10 cases in a cohort of rugby union players
This early resolution of symptoms may cause the frequency of early recurrences that has been described for this sub-type, with 76% of recurrences occurring within the first 3 months [13]. Incomplete aponeurotic healing remains at 6 weeks following injury [19], so perhaps one principle of management would be a more cautious approach with consideration of the stages of healing.
Periodisation of rehabilitation should give consideration to three keystones – (1) anatomical diagnosis, (2) functional diagnosis or limitations and (3) the demands of ‘return to sport’. Given the nature of the anatomical diagnosis in this case, and the risk of early recurrence, it is proposed that a gentler cadence through the process is best. As with the recommendations for intramuscular tendon injury [11], sprinting activities and exercises involving maximal length, high force and rate of loading should be programmed in a manner that respect immature histological healing at the location of injury.
Consideration should also be given to the distinct characteristics of the distal BF that could be implicated in the poor recovery from injuries in this location as identification of these directs the strength training interventions[20]. The proximal and middle regions of the BFlh have larger pennation angles and greater fascicle lengths than the distal portion [16]. Although this has not prevented the proximal hamstring from being more frequently injured, perhaps the shorter fascicle lengths of the distal hamstring are implicated in poor recovery when injury does occur. Similarly, the distribution of fibre types is not uniform throughout the muscle, with a greater proportion of type 2 muscle fibres existing proximally. This could impact upon the type of training that is deemed optimal for this region.
The duel innervation of the BF is consistently suggested as a potential reason for the high proportion of injuries to this muscle. Given T-junction injuries occur at the confluence of the two heads, it is logical that an asynchrony in co-ordination of the heads could contribute. However, how this can be quantified, and resolved, is unclear and it is only speculative as to what approach could be taken. Macdonald, McAleer [11] suggest isometric exercises as a tool to overcome the neuromuscular inhibition that exists during eccentric exercise following injury[21], and a similar approach may yield benefit in injuries at this confluence.
Recent research has demonstrated the differences in inter-muscular activation during various exercises [20], and has allowed for increasing specificity in rehabilitation. The ‘Nordic hamstring exercise’ and ‘single-leg hip extension’ elicit high activity in the biceps femoris muscle, and thus exercises with these characteristics should be considered important for eliciting an adaptation, while also treated with caution given they are likely to stress this area. Subsequently, Hegyi, Csala [22] has expanded upon this, by demonstrating region specific differences within individual muscles (Figure 3). The eccentric component of the straight knee bridge, upright hip extension conic-pulley and slide leg curl may be most appropriate if attempting to elicit a location specific response in this region, with contraction type adapted dependant on whether the goal is to overcome inhibition (isometric), develop fascicle length or local strength and hypertrophy (eccentric), or simply to induce healing through mechanotherapy. However, again, it is not known whether these injuries occur due to compensation for proximal dysfunction – at which point offloading distally would be the targeted outcome. In the absence of this information, a balanced programme is advised, giving cognisance to inter-muscular and proximal-distal biases, across multiple contraction types.
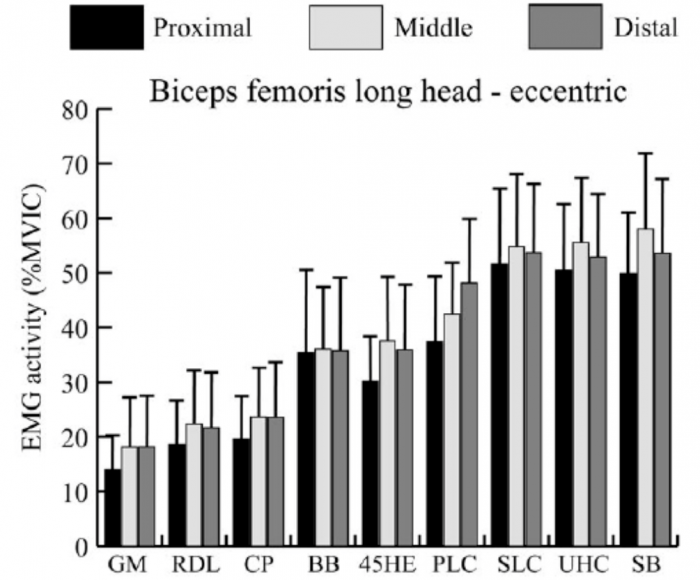
Figure 3: Reproduced from Hegyi, Csala [22]. Mean and standard deviation of the normalized activity level (%MVIC, maximal voluntary isometric contraction) in the proximal, middle, and distal regions of each muscle during the eccentric phase of each exercise. GM, good morning; RDL, unilateral Romanian deadlift; CP, cable pendulum; BB, bent‐knee bridge; 45HE, 45 degree hip extension; PLC, prone leg curl; SLC, slide leg curl; UHC, upright hip extension conic‐pulley; SB, straight‐knee bridge
Given that early recurrence is a key feature is this injury, the pace of progression is critical. If attempting to offload the distal BF, exercises that preferentially activate the medial hamstring or proximal BF may be indicated. In addition, initially restricting range of motion and rate of force development, as well as muscle length across the two involved joints are characteristics of exercise selections that can be manipulated and progressed, while still giving consideration to prioritising the adaptations that might be necessary to prevent recurrence (Table 4).
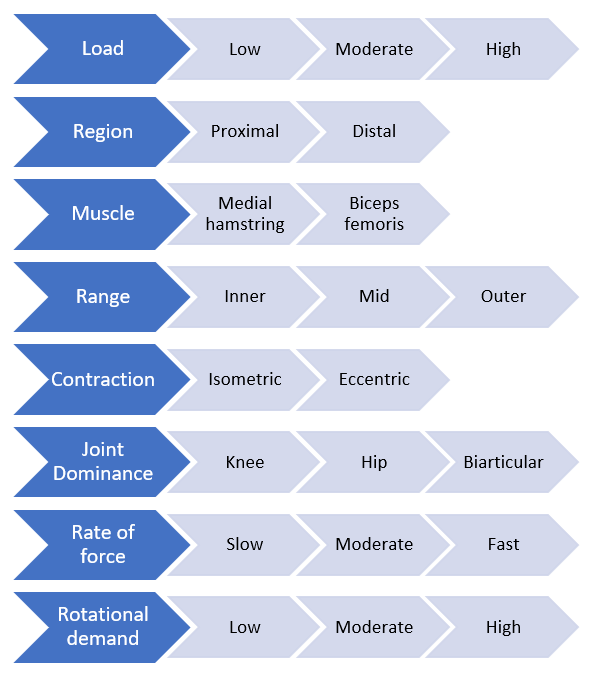
Figure 4: Proposed conceptual progressive loading model specific to a hamstring strain injury
In conclusion, it’s clear that an even more complete approach to rehabilitation is required following T-Junction than for a typical HSI, giving consideration to the structural diagnosis and characteristics of the distal BF. At present however, it remains unclear which anatomical and morphological traits have the greatest influence on injury risk, nor which approaches will generate the most specific and appropriate adaptation. In addition, strategies that help with the identification of these injuries and raise suspicion amongst clinicians would likely improve management of this complex variant of HSI.
References:
- Ekstrand, J., et al., Injury rates decreased in men's professional football: an 18-year prospective cohort study of almost 12 000 injuries sustained during 1.8 million hours of play. Br J Sports Med, 2021.
- de Visser, H.M., et al., Risk factors of recurrent hamstring injuries: a systematic review. Br J Sports Med, 2012. 46(2): p. 124-30.
- Koulouris, G., et al., Magnetic resonance imaging parameters for assessing risk of recurrent hamstring injuries in elite athletes. Am J Sports Med, 2007. 35(9): p. 1500-6.
- Pollock, N., et al., British athletics muscle injury classification: a new grading system. Br J Sports Med, 2014. 48(18): p. 1347-51.
- van der Made, A.D., et al., Intramuscular tendon involvement on MRI has limited value for predicting time to return to play following acute hamstring injury. 2018(1473-0480 (Electronic)).
- van der Made, A.D., et al., Intramuscular tendon injury is not associated with an increased hamstring reinjury rate within 12 months after return to play. 2018(1473-0480 (Electronic)).
- Pollock, N., et al., Time to return to full training is delayed and recurrence rate is higher in intratendinous ('c') acute hamstring injury in elite track and field athletes: clinical application of the British Athletics Muscle Injury Classification. Br J Sports Med, 2016. 50(5): p. 305-10.
- Eggleston, L., M. McMeniman, and C. Engstrom, High-grade intramuscular tendon disruption in acute hamstring injury and return to play in Australian Football players. Scand J Med Sci Sports, 2020.
- Comin, J., et al., Return to competitive play after hamstring injuries involving disruption of the central tendon. Am J Sports Med, 2013. 41(1): p. 111-5.
- Vermeulen, R., et al., Complete resolution of a hamstring intramuscular tendon injury on MRI is not necessary for a clinically successful return to play. Br J Sports Med, 2020.
- Macdonald, B., et al., Hamstring rehabilitation in elite track and field athletes: applying the British Athletics Muscle Injury Classification in clinical practice. Br J Sports Med, 2019. 53(23): p. 1464-1473.
- Askling, C.M., et al., Proximal hamstring strains of stretching type in different sports: injury situations, clinical and magnetic resonance imaging characteristics, and return to sport. Am J Sports Med, 2008. 36(9): p. 1799-804.
- Entwisle, T., et al., Distal Musculotendinous T Junction Injuries of the Biceps Femoris: An MRI Case Review. Orthop J Sports Med, 2017. 5(7): p. 2325967117714998.
- Kenneally-Dabrowski, C., et al., A retrospective analysis of hamstring injuries in elite rugby athletes: More severe injuries are likely to occur at the distal myofascial junction. Phys Ther Sport, 2019. 38: p. 192-198.
- Askling, C.M., et al., Acute first-time hamstring strains during high-speed running: a longitudinal study including clinical and magnetic resonance imaging findings. Am J Sports Med, 2007. 35(2): p. 197-206.
- Huygaerts, S., et al., Does Muscle-Tendon Unit Structure Predispose to Hamstring Strain Injury During Running? A Critical Review. Sports Med, 2021. 51(2): p. 215-224.
- Kayani, B., et al., Surgical Repair of Distal Musculotendinous T Junction Injuries of the Biceps Femoris. Am J Sports Med, 2020. 48(10): p. 2456-2464.
- Valle, X., et al., The MLG-R muscle injury classification for hamstrings. Examples and guidelines for its use. Apunts. Medicina de l'Esport, 2019. 54(202): p. 73-79.
- Jaspers, R.T., et al., Healing of the aponeurosis during recovery from aponeurotomy: Morphological and histological adaptation and related changes in mechanical properties. Journal of Orthopaedic Research, 2005. 23(2): p. 266-273.
- Bourne, M.N., et al., An Evidence-Based Framework for Strengthening Exercises to Prevent Hamstring Injury. Sports Med, 2018. 48(2): p. 251-267.
- Fyfe, J.J., et al., The role of neuromuscular inhibition in hamstring strain injury recurrence. J Electromyogr Kinesiol, 2013. 23(3): p. 523-30.
- Hegyi, A., et al., High-density electromyography activity in various hamstring exercises. Scand J Med Sci Sports, 2019. 29(1): p. 34-43.
- Hegyi, A., et al., Individual Region- and Muscle-specific Hamstring Activity at Different Running Speeds. Med Sci Sports Exerc, 2019. 51(11): p. 2274-2285.
The dream for many sportspeople is to forge a long and successful career as a full-time professional athlete. However, only very few are lucky enough to experience this, and many more athletes across the world end up showcasing their talents as a part-time or semi-professional athlete.
Rather than having the luxury of dedicating most of their time to training and recovery, these athletes are required to work full time jobs (often labour intensive), and then attend training sessions at the end of a 10 hour work day, with training loads very similar to that of an elite athlete.
This obviously poses a massive challenge to the athlete. Having to try and fit in work, training, recovery, family time, social time and sleep all in the space of a 24 hour day.
Managing these athletes can also be a massive challenge for the sports physiotherapists helping them to rehabilitate their injuries and keeping them out on the park.
As we know, load management is an integral part of progressing through a rehabilitation plan, and also helping to reduce the risk of any niggles or injuries. Over the past few years, even with limited resources at semi professional sporting organisations, physios and S+C staff have become much better at monitoring and analysing player loads from a physical, mental and emotional perspective. However, this is where the real challenge lies in dealing with players who work physical jobs throughout the day. For example, take a player who has suffered a calf strain 10 days ago. We can’t expect a player to tell us exactly how many times he has gone up and down the ladder during his work day as an electrician, but should this be a consideration in how much running he does at training that night?
For the athlete playing at this level, at the end of the day, their paid work is a higher priority for the majority of them over their ability to play sport. This often means that rehabilitation from an injury is compromised or lengthened in time, due to the pressures of having to return to work and feed their families. Take the athlete who has had an ACL reconstruction, but also works as a carpenter. The athlete will be eager to return to full time work as soon as they get the all clear from their surgeon, but will being on their feet all day and repetitively squatting cause a knee effusion that will then hinder their ability to perform and progress their strength work?
As their sport might not be their number one priority in their lives as mentioned, training consistency can also be a challenge in dealing with players at this level. Work and family commitments can sometimes clash with training sessions, with missed training sessions affecting their training load for that week, and potentially increasing their risk of injury in the coming weeks.
The emotional toll that having to fit so much into one day can take on the athlete, is also a vital consideration as a sports physiotherapist at this level. We are in a great position as sports physiotherapists to chat to players to ask them how they are coping. Whilst strapping their ankle, we can gain a lot of information about whether or not the athlete has a rough day or period or time, and whether or not they should have a lighter night on the track to help not overload their nervous system.
Many challenges and questions have been posed above, but the number one question is what can we as sport physiotherapists do to help semi-professional athletes overcome these challenges?
In my opinion, the best thing we can do here is to educate our athletes as much as possible, and focus on the ‘big-ticket’ items to allow them to stay at their best for as long as possible.
The ‘big-ticket’ items for me are:
- Sleep – As we know, sleep has been shown to be the most important recovery technique out there for athletes. Sleep is available to both professional and semi-professional athletes, so this has to be a priority.
- Importance of communication – Empower and encourage the athletes to communicate with coaches, S+C staff and physios so we can better monitor how they are dealing with the challenges of being a semi-professional athlete.
- Training consistency – Missing a 10km training session during the week and not making up for it, can often lead to an injury down the track from my experience. It is up to the S+C coach, physio and athlete to formulate a plan as to how to best make up for this session.
I am sure for those sport physiotherapists out there who work at this level with athletes, these are common challenges for you, along with many more that I have not mentioned. Because of these challenges, I find working with these athletes highly enjoyable and rewarding, and I hope you do too!